More Information
Submitted: March 06, 2022 | Approved: April 05, 2022 | Published: April 07, 2022
How to cite this article: Chaddad R, Rabah H, Awada B, Hmadeh M. Save the radial: go distally. J Cardiol Cardiovasc Med. 2022; 7: 026-029.
DOI: 10.29328/journal.jccm.1001128
Copyright License: © 2022 Chaddad R, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Save the radial: go distally
Rima Chaddad1*, Hussein Rabah2, Batoul Awada1 and Malek Hmadeh3
1Cardiology Fellow, Lebanese University, Beirut, Lebanon
2Internal Medicine, Staten Island University Hospital, Northwell Health, New York, USA
3Interventional Cardiologist, Beirut Cardiac Institute, Lebanon
*Address for Correspondence: Batoul Awada, Cardiology Fellow, Lebanese University, Beirut, Lebanon, Email: batoul.awada@outlook.com
Coronary artery disease is the leading cause of death worldwide.
Percutaneous coronary intervention (PCI) is one of the most widely performed medical procedures used to save lives, currently over 3 million annually worldwide.
The femoral artery has been the preferred vascular access site.
However, radial access is gaining extensive popularity due to the benefits of earlier ambulation, fewer access site complications, and decreased rates of bleeding.
Improvements in technology and understanding of the anatomic features of the vascular system have led to new insights into coronary angiography procedures.
Distal radial access, which was first used in 2017, shows a higher success rate and fewer complications than previous sites; therefore, it might be the future for cardiovascular intervention.
For this purpose, we conducted this prospective study at Beirut Cardiac Institute (BCI) comparing the two arms: radial vs. distal radial artery techniques through the anatomical snuffbox, in terms of patient’s length of stay, complication rate, and success rate of each procedure.
Access sites for coronary intervention have been evolving over the last decades. For many years, the common femoral artery had been the preferred access site for coronary angiography and angioplasty [1]. However, technological advancements, miniaturization of diagnostic catheters, and improvement of the equipment facilitating percutaneous transluminal coronary angioplasty have been increasing interest in the percutaneous arm approach via the radial artery [2,3].
Currently, the trans-radial approach (TRA) is the standard of care during percutaneous coronary intervention (PCI) [4], due to the lower complication rates, such as bleeding and blood transfusion, compared to the transfemoral approach, particularly during acute coronary syndrome (ACS) interventions [5]. In addition, TRA is associated with improved prognosis and quality of life (e.g., reduction in mortality rate, improvement in patient comfort after PCI, easy nursing at the ward, short hospital stay, reduction of cost, etc.) [6].
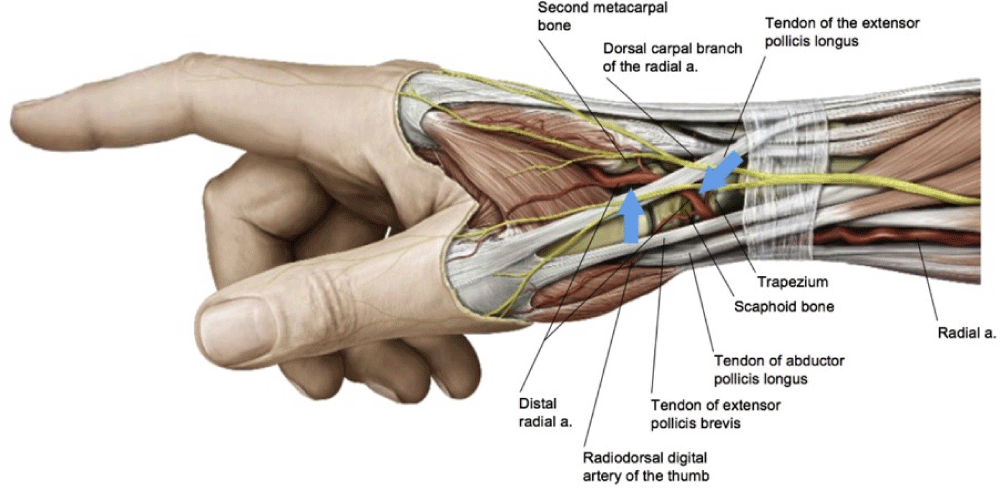
In 2017, Kiemeneij, et al. reported that radial artery cannulation through the anatomical snuffbox is safe and feasible [7] (Figure 1). Although such an approach shows higher success rates and fewer complications than other sites, there is not enough evidence to support its recommendation by the current guidelines.
Figure 1: Atlas of Human Anatomy (Netter Basic Science) 5th edition-plate 455.
Thus, the purpose of this study is to evaluate the safety and feasibility of radial artery access through the anatomical snuffbox by comparing its success rate, complication rate, and length of patients’ stays to the standard radial approach.
This prospective study included 100 patients admitted for percutaneous coronary interventions into Beirut Cardiac Institute, Lebanon, from June to September 2021. Approval to conduct this study was obtained from the IRB committee at the hospital. Patients were randomly assigned to the standard radial approach or distal radial approach. Consent was obtained from each patient or health care proxy before any interventions.
Inclusion criteria: All adult patients who underwent coronary procedures through radial or distal radial artery approach.
Exclusion criteria: Those who underwent other coronary procedures like cerebral angiography, carotid angiography, or lower limbs arteriography.
During the intervention, a successful procedure was defined as obtaining access through radial or distal radial with the complete procedure (from sheath insertion to wire crossing, catheter advancement, coronary cannulation, and smooth stent insertion in case of coronary interventions) through the same approach without major complications.
The primary endpoint of this study is to assess the success rate of the distal radial approach compared to the standard trans-radial approach.
Secondary endpoints include comparing the pain severity during the procedures, the number of attempts, and the length of stay for each approach.
Data collected include gender, age, indication for coronary intervention, approach (whether radial or distal radial), outcome, and pain during the procedure.
Data analysis
Statistical analysis was conducted using SPSS version 24.0 (Armonk, NY: IBM Corp). Age was presented as mean and standard deviation, while all the others were as frequencies and percentages. Comparative analysis was conducted comparing radial versus distal approach using the Chi-square test and Fisher’s exact test. Logistic regression was used to model predictive factors of outcome variables, including failure, the number of attempts, discharge, pain, and study the effect of radial and distal intervention as well as sex differences on such outcomes. Significance was interpreted based on confidence intervals and an alpha level below 0.05.
Studied population
In total, data from 100 patients were included in the study. Subjects were between 32 and 90 years old. The mean age was 61 +/- 10.8 years (Table 1). Overall, 38 (38%) were females, and 62 (62%) were males (Table 2).
| Table 1: Distribution of age. | |
| age | |
| N | 100 |
| Mean | 61.62 |
| Median | 61 |
| Std Deviation | 10.839 |
| Range | 60 |
| Minimum | 32 |
| Maximum | 92 |
| Table 2: Distribution of gender. | ||
| Frequency | Percent | |
| F | 38 | 38 |
| M | 62 | 62 |
| Total | 100 | 100 |
Indications
Indications for coronary interventions were Acute coro-nary syndrome including STEMI, chronic coronary syndrome including bypass graft angiography, pre-operative (valvular replacement), pre-alcohol septal ablation, or workup of heart failure with reduced ejection fraction, etc (Table 3).
| Table 3: Indications of the procedure. | ||
| Frequency | Percent | |
| HFrEF | 2 | 2.0 |
| valvular pre-op | 6 | 6.0 |
| NSTEMI | 25 | 25.0 |
| UA | 56 | 56.0 |
| stress test positive | 7 | 7.0 |
| STEMI | 3 | 3.0 |
| Preseptal alcohol | 1 | 1.0 |
| Total | 100 | 100.0 |
Outcomes
50 patients were treated using the standard radial approach, and 50 were treated using the distal radial approach with failing attempts in 10% and 14% of the procedures, respectively (p = 0.538) (Table 4). Furthermore, the second cannulation was attempted in 20% and 24% of patients in each group, respectively. However, the difference was statistically nonsignificant (p = 0.629) (Table 5).
| Table 4: Failure rate between radial/distal radial procedures. | ||||||
| Failed | Total | p | ||||
| no | yes | |||||
| Radial/distal | Distal | Count | 43 | 7 | 50 | 0.538 |
| % withinFailed | 48.90% | 58.30% | 50.00% | |||
| Radial | Count | 45 | 5 | 50 | ||
| % within Failed | 51.10% | 41.70% | 50.00% | |||
| Total | Count | 88 | 12 | 100 | ||
| % within Failed | 100.00% | 100.00% | 100.00% | |||
| Table 5: radial/distal radial, number of attempts crosstabulation. | ||||||
| Number of attempts | Total | p | ||||
| 1 | 2 | |||||
| Radial/distal | Distal | Count | 38 | 12 | 50 | 0.629 |
| % within Radial/distal | 76.00% | 24.00% | 100.00% | |||
| Radial | Count | 40 | 10 | 50 | ||
| % within Radial/distal | 80.00% | 20.00% | 100.00% | |||
| Total | Count | 78 | 22 | 100 | ||
| % within Radial/distal | 78.00% | 22.00% | 100.00% | |||
Females had 3.87 higher odds of failure (p < 0.001, CI {1.08, 13.89} in both proximal and distal groups, in addition to having 6.8 times higher odds of requiring sedation than males (p = 0.001, OR = 6.8, CI {2.22,20.69}.
Pain severity
14% of the patients experienced severe pain during both proximal and distal approaches, while 22% had mild pain during the distal approach compared to 10% during the proximal approach. The pain was absent during distal and proximal approaches in 64% and 76% of the interventions, respectively (p = 0.251) (Table 6).
| Table 6: Pain scale in both groups. | |||||||
| Pain | Total | p - value | |||||
| None | Mild | Severe | |||||
| Radial/distal | Distal | Count | 32 | 11 | 7 | 50 | 0.251 |
| % within Radial/distal | 64.00% | 22.00% | 14.00% | 100.00% | |||
| Radial | Count | 38 | 5 | 7 | 50 | ||
| % within Radial/distal | 76.00% | 10.00% | 14.00% | 100.00% | |||
| Total | Count | 70 | 16 | 14 | 100 | ||
| % within Radial/distal | 70.00% | 16.00% | 14.00% | 100.00% | |||
Time for discharge
Three hours after the procedure, 31 patients (62%) of the patients who underwent distal intervention were discharged, compared to none with proximal intervention. On the other hand, most of the patients who had proximal radial approach (74%) coronary angiography were discharged after 6 hours of the procedure. The rest of the patients were discharged after 24 hours of the procedure (p < 0.001) (Table 7).
| Table 7: Discharge hours in both groups. | |||||||
| Discharge | total | p - value | |||||
| 3 hours | 6 hrs | 2 days | |||||
| Radial/diastal | Distal | Count | 31 | 3 | 16 | 50 | |
| % within distal | 62% | 6.00% | 32% | 100% | |||
| radial | count | 0 | 37 | 13 | 50 | < 0.001% | |
| % within radial | 0.00% | 74% | 26% | 100% | |||
| Total | count | 31 | 40 | 29 | 100 | ||
| % within radial/distal | 31% | 40% | 29% | 100% | |||
Anatomy
In the cubital fossa, the brachial artery bifurcates into the ulnar artery and the radial artery, providing a dual vascular supply to the hand.
The radial artery descends along the lateral side of the forearm above the radius toward the wrist, where it is palpable between the tendon of the flexor carpi radialis medially and the anterior border of the radius.
The anatomical snuffbox is defined as a triangular depression on the dorsum of the hand at the base of the thumb; it is bordered by the abductor pollicis longus and extensor pollicis brevis laterally and the extensor pollicis longus medially. The floor is formed by the scaphoid and trapezium carpal bones (Figure 1).
There are two sites at which the radial pulse can be found: in the anatomic snuffbox and the first intermetacarpal space; these two sites represent alternative puncture points for DRA [6].
Once it has reached the anatomic snuffbox or the dorsum of the hand, the radial artery has already given rise to some branches that, in case of vessel occlusion occurring at the distal radial artery puncture site, could avoid flow interruption in the forearm radial artery and possibly limit the reduction of blood supply to the hand. Flow interruption appears to play a central mechanism in the complex interplay of factors leading to radial artery occlusion [8].
In this background, DRA could maintain forearm radial artery patency during hemostatic compression or in case of occlusion at the puncture site [9].
It is essential to know that the DRA diameter is 20% less than the proximal [10].
In 2018, Kiemeneij, et al. reported a success rate of 89% using the DRA [11]. Subsequently, different studies described highly successful rates ranging between 88% and 99.5% [12]. Such results are similar to those observed in this study, with a success rate of 86%.
On the other hand, a two-center study conducted by Ziakas, et al. on 49 patients reported 10.2% failed attempts while utilizing DRA [13], which is slightly lower than that concluded by our study (14%). The most common etiologies behind the failure of the DRA include puncture failure, hypoplastic/vasospastic distal radial artery, followed by failure to advance the guidewire [14].
Hammami et al showed in their study on 177 patients, a success rate of 98% for the RA group and 88% for the DRA group (p = 0.008) [15].
In this report, RA interventions had a slightly higher success rate than DRA (90% and 84%, respectively). However, this difference was statistically nonsignificant (p = 0.538). The familiarity with the proximal radial access, which is the most common access used. In our center, 95% of the coronary procedures were done through radial access, the remaining through the femoral approach, and this could explain such a nonstatistical difference.
In addition, females had 3.8 higher odds of procedure failure and 6.8 higher odds of requiring sedation during both DRA and RA interventions compared to males and this difference may be contributed to lesser radial artery diameter in females compared to males proved by T. Asharaf where the mean diameter of radial arteries in males was 2.3 ± 0.39 mm in comparison to females 2.11 ± 0.29 mm (p - value < 0.05) [16].
On the other hand, research shows that complications occurred in 2.4% of DRA procedures, of which bleeding/hematoma (18.2%) were the most frequent [15]. Some cases of dissection and arterio-venous fistulation had been reported.
In our study, no complications were reported using both access sites, and there was no statistically significant difference in the degree of pain expressed by the patients (p - 0.251). Therefore, DRA is an efficient and safe approach during coronary angiography.
Furthermore, most patients with a dRA access site (67%) were discharged 3 hours earlier than patients with the RA approach. The reason behind this is the superficial location of DRA that could make hemostasis easier and faster.
Coronary artery catheterization is utilized for stable coronary artery disease (including patients with bypass grafts) diagnosis and treatment, open heart surgery pre-operative assessment, and revascularization of patients with acute coronary syndromes. Patients with bypass grafts (especially LIMA and RIMA grafts) need to obtain 2 access sites left and right if performed via radial or distal radial approach.
It is crucial to intervene promptly during an ACS to prevent further myocardial ischemia and this was successfully achieved using the dRA. Hence, dRA cannulation can be attempted in almost all patients who have an indication for coronary angiography, including ACS.
Limitations: All procedures were done in the same center.
Distal radial artery cannulation is an efficient and reliable intervention to approach patients with various acute and chronic heart conditions. It appears to be a safe and feasible procedure. Further larger randomized trials are still needed to assure the safety and the benefits of this coronary intervention technique.
We gratefully thank our Beirut Cardiac Institute, Cath Lab team including cardiologists and technicians especially Mr. Abbas Deoun who helped us to finalize our study, and his professional team (Mr. Mahmoud Saleh, Mr. Hussein Rida, Mr. Mohamad Bachir and Mr. Amer Haidar) for their valuable efforts.
- Helfrich CD, Tsai TT, Rao SV, Lemon JM, Eagenis EC, et al. Perceptions of advantages and barriers to radial access percutaneous coronary intervention in VA cardiac catheterization laboratories. Cardiovasc Revasc Med. 2014; 15: 329-333. PubMed: https://pubmed.ncbi.nlm.nih.gov/25282521/
- Amoroso G. Transradial approach for percutaneous coronary interventions: the future is now. Interventional Cardiol. 2013; 5: 279-288.
- Archbold RA, Robinson NM, Schilling RJ. Radial artery access for coronary angiography and percutaneous coronary intervention. BMJ. 2004; 329: 443–446. PubMed: https://pubmed.ncbi.nlm.nih.gov/15321904/
- Kiemeneij F, Laarman GJ. Percutaneous transradial artery approach for coronary stent implantation. Catheter Cardiovasc Diagn. 1993; 30: 173–178. PubMed: https://pubmed.ncbi.nlm.nih.gov/8221875/
- Valgimigli M, Gagnor A, Calabró P, Frigoli E, Leonardi S, et al. Radial versus femoral accessin patients with acute coronary syndromes undergoing invasive management: a randomised multi-centre trial. Lancet. 2015; 385: 2465–2476. PubMed: https://pubmed.ncbi.nlm.nih.gov/25791214/
- Lee CW, Cho SC. The Transradial Approach for Coronary Intervention: More Comfort, Better Outcome. Korean Circ J. 2018; 48: 728–730. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6072665/
- Nairoukh Z, Jahangir S, Adjepong D, Malik BH. Distal Radial Artery Access: The Future of Cardiovascular Intervention. Cureus. 2020; 12: e7201. PubMed: https://pubmed.ncbi.nlm.nih.gov/32269880/
- Sgueglia GA, Di Giorgio A, Gaspardone A, Babunashvili A. Anatomic Basis and Physiological Rationale of Distal Radial Artery Access for Percutaneous Coronary and Endovascular Procedures. JACC: Cardiovasc Interv. 2018; 11: 2113–2119. PubMed: https://pubmed.ncbi.nlm.nih.gov/30336816/
- Corcos T. Distal radial access for coronary angiography and percutaneous coronary intervention: a state-of-the-art review. Catheter Cardiovasc Interv. 2019; 93: 639-644. PubMed: https://pubmed.ncbi.nlm.nih.gov/30536709/
- Sgueglia GA, Di Giorgio A, Gaspardone A, Babunashvili A. Anatomic basis and physiological rationale of distal radial artery access for percutaneous coronary and endovascular procedures. JACC Cardiovasc Interv. 2018; 11: 2113-2119. PubMed: https://pubmed.ncbi.nlm.nih.gov/30336816/
- Kaledin AL, Kochanov IN, Podmetin PS, Seletsky SS, Ardeev VN. Distal radial artery in endovascular interventions. ARYA Atheroscler. 2018; 14: 95-100.
- Lee JW, Park SW, Son JW, Ahn SG, Lee SH. Real-world experience of the left distal transradial approach for coronary angiography and percutaneous coronary intervention: a prospective observational study (LeDRA). EuroIntervention. 2018; 14: e995-e1003. PubMed: https://pubmed.ncbi.nlm.nih.gov/30222122/
- Ziakas A, Koutouzis M, Didagelos M, Tsiafoutis I, Kouparanis A, et al. Right arm distal transradial (snuffbox) access for coronary catheterization: Initial experience. Hellenic J Cardiol. 2020; 61: 106-109. PubMed: https://pubmed.ncbi.nlm.nih.gov/30389385/
- Aqel R, Alzughayyar T, Misk R. Radial: time to go distal. Cardiol Cardiovasc Med 2019; 3: 432-437.
- Hammami R, Zouari F, Ben Abdessalem MA, Sassi A, Ellouze T, et al. Distal radial approach versus conventional radial approach: a comparative study of feasibility and safety. Libyan J Med. 2021; 16: 1830600. PubMed: https://pubmed.ncbi.nlm.nih.gov/33147107/
- Asharaf T, Panhwar Z, Habib S, Memon MA, Shamsi F, et al. Size of radial and ulnar artery in local population. J Pak Med Assoc. 2010; 60: 817-819. PubMed: https://pubmed.ncbi.nlm.nih.gov/21381609/