More Information
Submitted: 01 November 2019 | Approved: 14 November 2019 | Published: 15 November 2019
How to cite this article: Bagchi A, Agarwal RK, Talwar KK. Hemoptysis after subclavian vein puncture for pacemaker implantation: A case report. J Cardiol Cardiovasc Med. 2019; 4: 192-194.
DOI: 10.29328/journal.jccm.1001065
ORCiD: orcid.org/0000-0002-7879-2680
Copyright License: © 2019 Bagchi A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Case report; Subclavian venous access; Alveolar hemorrhage; Hemoptysis; Chest x-ray
Hemoptysis after subclavian vein puncture for pacemaker implantation: A case report
Avishek Bagchi1, Rajendra Kumar Agarwal2 and Kewa1 Kishan Talwar3*
1Associate Consultant, Max Super Speciality Hospital, Saket, New Delhi, India
2Consultant, Max Super Speciality Hospital, Saket, New Delhi, India
3Chairman, Cardiology, Max Healthcare, New Delhi, India
*Address for Correspondence:Talwar KK, Chairman, Cardiology, Max Super Specialty Hospital, 1 & 2, Press Enclave Marg Saket District Centre Saket Institutional Area, Saket, New Delhi, India, Tel: +91-8800232211; Email: kktalwar@hotmail.com
Background: Subclavian venous access for pacemaker lead insertion is a common procedure and is normally considered safe in the hands of an expert. However, subclavian venepuncture is not without complications, starting from mild subcutaneous hematoma to pneumothorax. We here present a case of hemoptysis occurring after difficult subclavian vein puncture, which subsequently improved on conservative management only.
Case Summary: A 65-year-old gentleman, post aortic valve replacement had persistent high-grade AV block and was taken up for a dual chamber pacemaker implantation. Immediately following venous access, he had a bout of hemoptysis, which recovered on its own. Post procedure chest x-ray was suggestive of alveolar hemorrhage which cleared gradually in next three-four days.
Discussion: Post subclavian venepuncture hemoptysis is known; but it is a rare complication, arising either because of lung parenchyma injury or arterial injury. This is mostly benign and improves on conservative management only; however rarely it may be massive and life threatening where transcatheter arterial embolization may be required.
Subclavian vein puncture for accessing right heart is a common procedure and is normally considered safe in the hands of an expert. It has been the usual approach for endocavitary pacemaker lead placement since the early days [1,2]. However, subclavian venepuncture is not without complications, starting from mild subcutaneous hematoma to pneumothorax. Haemorrhagic complications like alveolar hemorrhage, hemothorax and hemoptysis are rare with subclavian venepuncture (0.1%) [3] and even though the course of these complications is usually benign and self-limited, there may be a severely adverse out¬come in critically ill patients [4]. We here present a case of hemoptysis occurring after difficult subclavian vein puncture, which subsequently improved on conservative management only. We also propose possible ways of minimizing such complications.
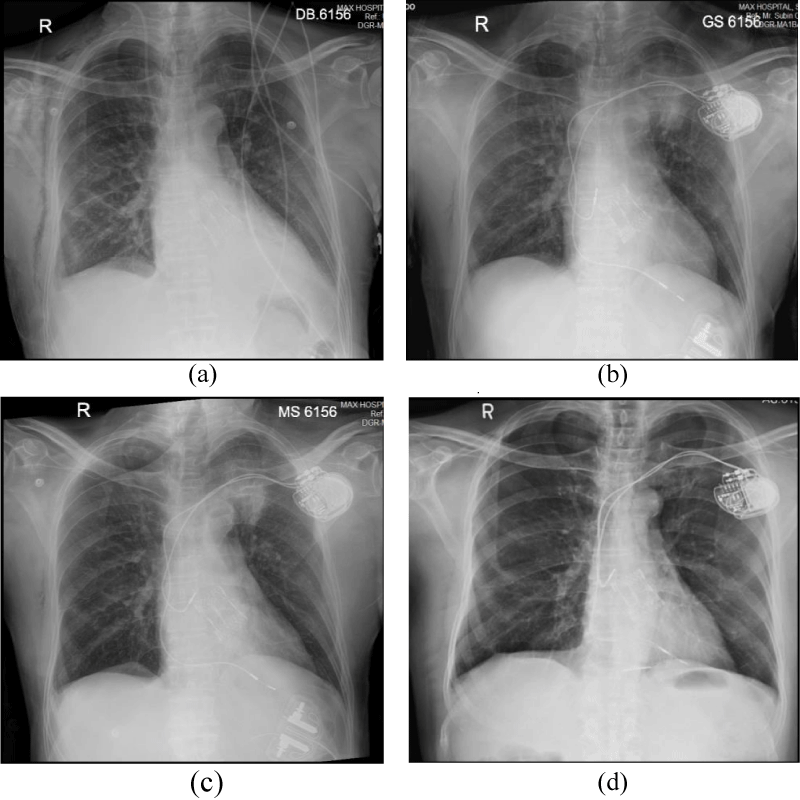
A 65-year-old man was admitted to our hospital with severe aortic stenosis for aortic valve replacement. He underwent aortic valve replacement with (#25/27 mm) XL sorin perceveal sutureless aortic valve prosthesis (bioprosthesis). Following the procedure, he developed high grade AV block which did not improve on two weeks; hence he was planned for a permanent dual chamber (DDD) pacemaker implantation. He was on low molecular heparin (enoxaparin 0.6 ml subcutaneous twice a day) and received the last dose of enoxaparin the last evening before the pacemaker implantation. However, he had a normal haemoglobin, platelet count and his INR was 1.1. His pre-procedure chest x-ray had normal lung parenchyma (Figure 1a).
Figure 1: (a) Pre procedure chest x-ray, (b) Immediate post procedure x-ray showing alveolar haemorrhage, (c) post procedure x-ray after one day showing clearance of lung parenchyma; (d)post procedure x-ray after 72 hours showing almost complete normalization.
We used left subclavian vein puncture, which is our preferred technique for venous access. The operator had almost 40 years of experience in cardiac pacing including experience in subclavian venepuncture even in young children for pacemaker implantation [5]. The infraclavicular approach based on anatomic landmarks was used without the use of ultrasonographic guidance, which is the usual practice of the operator. Left subclavian vein access was attempted with an 18-gauge needle, two tear-away introducer 7 Fr sheaths, and two flexible guidewires (0.035 in) with a J-shaped soft tip. The fluoroscopic guidance for guidewire navigation was used. Venous access was hard, and after two initial failed attempts, the operator had to shift a little medially and finally he got the venous access with blood return. A guidewire was inserted, the needle was removed, and the dilator was advanced. Immediately after the sheath insertion the patient had bouts of cough and around 50 ml of hemoptysis. However, his saturation did not fall, fluoroscopically his chest looked normal and there was no evidence of pneumothorax. There was no established evidence of arterial puncture or needle-air reflux suggesting a parenchymal puncture. With the guidance of the first puncture the second puncture was done rather quickly, sheath was introduced. Right ventricular and right atrial leads were placed, and good parameters were obtained. The procedure went quite smoothly after the initial attack of hemoptysis and the patient was asymptomatic in the immediate post-procedure period.
However, immediate post procedure chest x-ray showed left upper lobe homogenous opacities suggestive of alveolar haemorrhage with no evidence of pneumothorax (Figure 1b). We initially planned for a CT scan of thorax, but he improved and had no significant hemoptysis after the initial bout of hemoptysis in the Cath-lab. There was no drop in hemoglobin or no documented episode of hypoxia either. His subsequent chest x-rays showed clearance of the opacities (Figure 1c) and finally at fourth post procedure day, he was started on oral anticoagulation, chest x-ray became normal (Figure 1d) and he was discharged.
Subclavian vein puncture is a relatively fast and safe technique to access the right heart for placement of pacemaker leads. It has been used since the beginning of the era of endocavitary pacemaker lead placement [1,2] and has often been the preferred access technique for many operators. When we did a literature review, we found few cases where there was bleeding immediately after pacemaker insertion [4,6-12]. Some of these cases had only minor haemoptysis [4,6,8] as in our case, but few had significant pulmonary haemorrhage causing hemothorax [11] or requiring transcatheter arterial embolization for pulmonary artery injury [12].
There are two potential possibilities of such hemoptysis- lung parenchymal injury, as demonstrated by Yelgec, et al. [11], or arterial injury, either subclavian artery itself or one of its branches. Somsse have speculated that the puncture needle may create a fistulous tract between a small blood vessel and a bronchus and it can cause persistent minor hemoptysis [7].
The course is usually benign when the mechanism is injury of lung parenchyma, but it can be critical when the subclavian artery is lacerated along with parenchymal injury with potential formation of a track or fistula that maintain blood leak and hemoptysis [7].
How to predict such injury and how can one prevent it? As our patient was post valve replacement, he was on low molecular weight heparin, it may have exacerbated the injury. Secondly, in a post-surgical patient, there is always a possibility of some anatomic alterations which might have made venepuncture difficult even for an experienced operator. At the same time, because of initial difficulty the operator had to go more medially, which might have caused parenchymal lung injury. Puncture can be difficult in cases of anatomic alterations due to atypical subclavian vessels trajectory, atypical clavicular bone anatomy and/or atypical structure of the lungs (i.e., emphysema); also, in hypotensive or hypoxemic patients, arterial puncture may be mistaken for venous puncture.
For prevention, people have described venogram guided [13] or wire guided [4] venepunctures in difficult cases. However, venogram-guided method gives only transient guiding landmark and can be limited in case of renal failure or intolerance to the contrast product. Some authors have advocated extra-thoracic axillary venous puncture, but it is technically more challenging and has its own demerits [14]. Ultrasound guidance has also been described and is commonly used by some operators. However, it largely depends upon operator skill and experience; it is mostly a blind procedure and one should be careful. In case of such bleeding, one should not panic and manage properly. Though not done in our case as the patient improved on his own and the bleeding was only minor, a timely contrast CT scan may be done in cases where bleeding is significant.
Alveolar hemorrhage is a rare complication of subclavian vein puncture, and the course is usually benign but can be critical in patients with chronic lung disease or with coagulation disorders.
The authors confirm that written consent for submission and publication of this case report including images has been obtained from the patient in line with COPE guidance.
- Solomon N, Escher DJ. A rapid method for insertion of the pacemaker catheter electrode. Am Heart J. 1963; 66: 717–718. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/14083795
- McNeill GP, Taylor NC. Use of subclavian vein for permanent cardiac pacing. Br Heart J. 1978; 40: 114–116. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/637961
- Kirk AJ, Turner MA. Surgical aspects of permanent cardiac pacemakers. Life Support Syst. 1987; 5: 223–231. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/3695582
- Kossaify A, Nicolas N, Edde P. Hemoptysis after subclavian vein puncture for pacemaker implantation: importance of wire-guided venous puncture. Clin Med Insights Case Rep. 2012; 5:119-122. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22859867
- Talwar KK, Agarwal R, Rao YV. Permanent pacing by percutaneous subclavian vein in small children. Am Heart J. 1991; 122: 1796. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/1957790
- García-Anguiano Duque F, Marchena Gómez J, Servent Pedescoll R. Hemoptysis, a rare complication of punction-catheterization of the subclavian vein. Rev Clin Esp. 1994; 194: 202. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8008962
- Goldberg A, Inna Rosenfeld I, Marmor A. Hemoptysis—a rare complication of pacemaker implantation. Indian Pacing Electrophysiol J. 2008; 8: 75-76. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18270606
- Antonelli D, Atar S, Bloch L. Hemoptysis after subclavian vein puncture. Harefuah. 2007; 146: 744. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17990384
- Truong AT, Brown DL. Catastrophic hemothorax from lobar pulmonary artery puncture during attempted subclavian vein catheterization: the fallibility of venous blood aspiration. J Clin Anesth. 2009; 21: 377-378. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19700295
- Holt S, Kirkham N, Myerscough E. Haemothorax after subclavian vein cannulation. Thorax. 1977; 32: 101-103.
- Yelgec NS, Osken A, Turkkan C, Alper AT. Subclavian vein puncture-induced massive pulmonary hemorrhage and hemoptysis during pacemaker implantation. North Clin Istanb. 2018; 5: 254-255. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30688923
- Tokue H, Tokue A, Morita H, Yoshito T. Successful Interventional Management for Pulmonary Arterial Injury Secondary to Pacemaker Implantation. Case Rep Cardiol 2016; 2016:1–3. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/27882248
- Dora SK, Kumar VK, Bhat A, Tharakan JA. Venogram-guided extrathoracic subclavian vein puncture. Indian Heart J. 2003; 55:637-640. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/14989516
- Burri H, Sunthorn H, Dorsaz PA, Shah D. Prospective study of axillary vein puncture with or without contrast venography for pacemaker and defibrillator lead implantation. Pacing Clin Electrophysiol. 2005; 28 Suppl 1: S280-283. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15683516