Case Report
Single Trans apical access for double aortic and mitral valves-in-valves procedures with high risk of thrombus embolism

Julien Adjedj*, Mathias Kirsch, Anna Nowacka and Olivier Muller
Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland
*Address for Correspondence: Julien Adjedj, Centre Hospitalier Universitaire Vaudois, 1004 Lausanne, Switzerland, Tel: +41795560950; Email: julien.adjedj@chuv.ch
Dates:Submitted: 27 June 2019; Approved: 15 July 2019; Published: 16 July 2019
How to cite this article:Adjedj J, Kirsch M, Nowacka A, Muller O. Single Trans apical access for double aortic and mitral valves-in-valves procedures with high risk of thrombus embolism. J Cardiol Cardiovasc Med. 2019; 4: 071-072. DOI: 10.29328/journal.jccm.1001042
Copyright License: © 2019 Adjedj J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Valves in valves; Apical access; Right ventricle laceration
Abstract
Persistent left atrial thrombus remains a contra indication to transeptal valves in valves procedure. We aimed to perform a double valves in valves replacement through transapical access with cerebral angiography control during the procedure just after implantation. Our case shows the feasibility of this strategy and the management of right ventricle laceration successfully treated after extra corporeal membrane oxygenation implantation and local hemostasis. We reported a feasibility case report of successful double valves in valves implantation through transapical access with 6 months of clinical and computed tomography follow up.
Introduction
Double valves in valves replacement through single transapical access has been demonstrated has feasible in selected cases. However, patients with Trans septal access contraindication due to left atrial persistent thrombus remain poorly described. We aimed to perform a double valves in valves replacement with control of cerebral angiography in case of urgent thrombectomy.
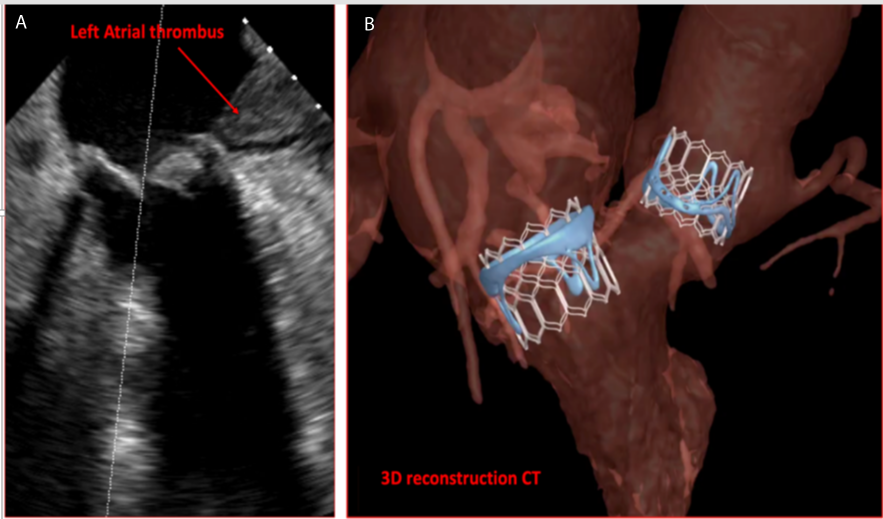
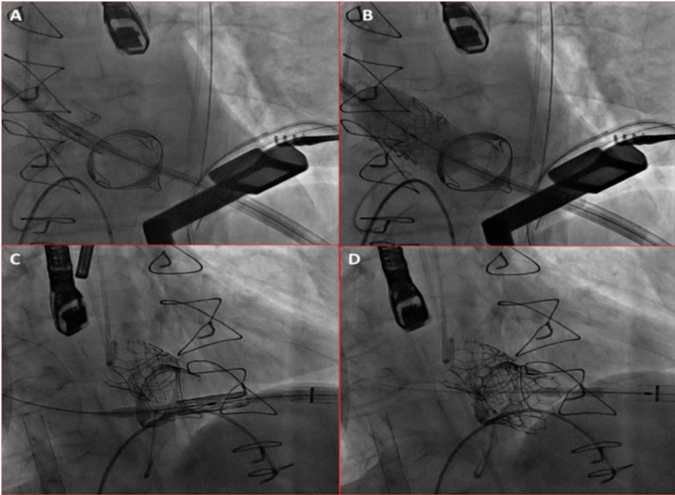
We report a 72 years old male patient case with past history of surgical aortic and mitral biological valves replacement with tricuspid ring in 2010. The patient presented severe dyspnea New York Heart Association (NYHA) class IV with stenotic aortic and mitral bio prostheses and left ventricle ejection fraction of 30%. The patient had no cardiovascular risk factor and received vitamin K antagonist (VKA) for persistent atrial fibrillation. Trans esophageal echocardiography (TEE) showed a severe aortic bioprosthesis stenosis with a mean aortic gradient of 32 mmHg, the estimated surface was 0.6 cm2 and a severe mitral bioprosthesis stenosis with a mean gradient of 20 mmHg, the estimated surface was 0.9 cm2 and pulmonary hypertension of 65 mmHg. TEE revealed the presence of a voluminous thrombus appended in the left atrium despite optimal anticoagulation (target INR stable between 2-3). The patient was screened for a double valves in valves procedure, coronary angiogram did not reveal significant coronary stenosis. We repeated the TEE after one month with the ad of aspirin on top of VKA to reduce the left atrial thrombus without success (Figure 1A). Heart team decision was to perform valves in valves (VIV) aortic and mitral replacement via transapical access due to the contra indication to use the transeptal access for the mitral bioprosthesis VIV. We planned this procedure with cardiac computed tomography (CT), 3-dimension reconstruction and VIV implantation simulation (Figure 1B). To rule out the high risk of stroke emboly during the procedure we involved interventional neurologist to perform cerebral angiography just after VIV implantations. The procedure was performed under general anesthesia with arterial femoral access 6F and venous femoral access 7F to introduce a temporary pacemaker. The transapical access was complicated with right ventricle laceration an urgent peripheral arteriovenous extracorporeal membrane oxygenation (ECMO) was implanted to unload the right ventricle and perform the hemostasis with success. Thereafter, we performed first a VIV implantation with an Edwards Sapien n°3 26 mm in aortic position and VIV implantation with an Edwards Sapien n°3 29 mm in mitral position without complication (Figure 2). Cerebral angiography did not showed occlusion of main cerebral arteries. ECMO was removed the same day and patient was discharged at home after 14 days relief of symptoms and without adverse neurological outcome. At 6 months follow up, patient was asymptomatic with stable mean gradients of 11 mmHg for the aortic VIV and 7 mmHg for the mitral VIV, left ventricle ejection fraction was 45%. Controlled CT showed thrombus regression and 3-dimension reconstruction was similar to the simulation.
Figure 1: A: Tran’s esophageal echocardiography showing left atrial thrombus. B: 3 dimension cardiac computed tomography reconstruction with valve in valve implantation simulation.
Figure 2: VIV procedure A: Trans aortic VIV positioning B: Tran’s aortic VIV deployment C: Trans mitral VIV positioning D: Tran’s mitral VIV deployment
Discussion
Our case report hence several discussion points. Albeit, Ando et al. [1] reported 11 double VIV with transapical access were reported with a good success rate. We reported to our knowledge for the first time in this procedure transapical complication with right ventricle laceration the ECMO implantation to unload the right ventricle and perform successful hemostasis. Right ventricle perforation could be due to the right ventricle dilatation and the pulmonary hypertension. The Apical access fragilized the apical right ventricle part which degenerated by a laceration. We did not have access to cerebral protection device in our institution, therefore we had the collaboration of interventional neurologist to perform cerebral angiography and in case of occlusion of main cerebral artery perform an embolectomy just after the VIV implantation. Transaortic Valve replacement (TAVI) reported a clinical stroke rate of approximately 3% [2]. TAVI under general anesthesia are at risk to underestimate per procedural stroke while cooperation with interventional neurologist could directly perform a thrombectomy of main cerebral arteries in case of clinical stroke or rule out stroke by performing just after the implantation a cerebral angiography in high risk patients with procedure performed under general anesthesia. Furthermore, in case of stroke most of our TAVI patients are contra indicated to thrombolysis and the nature of the emboli may suggest that thrombolysis will not be an effective treatment in all per procedural stroke during TAVI procedure [3]. Our case showed the feasibility of transapical double VIV procedure in high embolism risk with a heart team extended to interventional neurologist and the successful management of right ventricle successful hemostasis after laceration by using a bail out ECMO implantation.
References
- Ando T, Takagi H, Briasoulis A, Telila T, Slovut DP, et al. A systematic review of reported cases of combined transcatheter aortic and mitral valve interventions. Catheter Cardiovasc Interv. 2018; 91: 124-34. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28862381
- Eggebrecht H, Schmermund A, Voigtländer T, Kahlert P, Erbel R, et al. Risk of stroke after transcatheter aortic valve implantation (tavi): A meta-analysis of 10,037 published patients. EuroIntervention. 2012; 8: 129-38. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22391581
- Gülker JE, Schott P, Katoh M, Bufe A. Case report: Cerebral stentretreiver thrombectomy of an embolized valve fragment after valve in valve tavi. Clin Res Cardiol 2016; 105: 372-5. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26514354