Research Article
Design and validation of an Index to predict the development of Hypertensive Cardiopathy

Alexis Álvarez-Aliaga1*, Andrés José Quesada-Vázquez2, Alexis Suárez-Quesada3 and David de Llano Sosa4
1Specialist in Internal Medicine. Professor and Researcher, Carlos Manuel de Céspedes” General University Hospital and teach at Granma University of Medical Sciences, Cuba2Specialist in Internal Medicine. Professor and Researcher, Carlos Manuel de Céspedes” General University Hospital and teach at Granma University of Medical Sciences, Cuba
3Specialist in Internal Medicine. Instructor, Carlos Manuel de Céspedes” General University Hospital and teach at Granma University of Medical Sciences, Cuba
4Specialist in Internal Medicine. Professor and Researcher, Carlos Manuel de Céspedes” General University Hospital and teach at Granma University of Medical Sciences, Cuba
*Address for Correspondence: Alexis Álvarez Aliaga, Professor, MD, PhD, Carlos Manuel de Céspedes General University Hospital, Bayamo, Granma, Cuba, Tel: 23483034; 53085257; Email: alexis.grm@infomed.sld.cu
Dates: Submitted: 31 January 2018; Approved: 14 Febraury 2018; Published: 16 Febraury 2018
How to cite this article: Álvarez-Aliaga A, Quesada-Vázquez AJ, Suárez-Quesada A, de Llano Sosa D. Design and validation of an Index to predict the development of Hypertensive Cardiopathy. J Cardiol Cardiovasc Med. 2018; 3: 008-022. DOI: 10.29328/journal.jccm.1001022
Copyright License: © 2018 Álvarez-Aliaga A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction: The high morbidity and mortality by hypertensive cardiopathy demand the construction and validation of tools to stratify the risk of developing this condition.
Objective: To design and validate an index, based on risk factors, that permits to predict the development of hypertensive cardiopathy in patients with a diagnosis of essential arterial hypertension.
Methods: A prospective cohort study was done in hypertensive patients assisted at the specialized arterial hypertension physicians’ office of the “Carlos Manuel de Céspedes” Specialty Policlinic attached to the General University Hospital, Bayamo Municipality, Granma Province, Cuba from January 1st, 2010 to December 31, 2016. Internal and external validity and the internal consistency of the index were determined.
Results: The index sensitivity was of 97, 20 (IC: 93, 93-94.09) and specificity of 65, 38 (IC: 76, 25-76, 20). Both the index discriminative capacity (area under the ROC curve= 0,944; interval of confidence: 0.932-0.956; p<0.0005) and calibration (p=0.751) were adequate.
Conclusions: The present study proposes an index to predict the risk of developing hypertensive cardiopathy, with adequate discriminative capacity and calibration (external validity). The index can be used as a tool of clinical and epidemiological surveillance since it permits to identify subjects with greater probability of developing the condition and to stratify the risk.
Introduction
Arterial hypertension (HTN) has a high prevalence in the population in general and, in particular, in individuals over 60 year s of age of both sexes; it is one of the major risk factors for the development of heart disease, so its control is considered one of the most important measures to prevent diseases [1]. In Cuba the prevalence of HTN in the year 2016 was 219.4 per 1000 inhabitants 171 in Granma province [2]. HTN cannot be seen as an isolated condition because, due to its natural evolution, it increases considerably the risk of damage to different organs; as well as incapacity and death of cardiovascular cause [1,3].
Hypertensive cardiopathy is the damage to target organs caused by HTN which produces greater morbidity and mortality. It is defined as a complex and variable combination of effects which provokes a chronic elevation of the arterial blood pressure in the heart and is characterized by anatomical and biochemical signs of left ventricular hypertrophy or diastolic or systolic ventricular dysfunction, myocardial ischemia and cardiac rhythm alterations [4].
The importance of the hemodynamic overload that causes HTN in the development of cardiomyocyte hypertrophy is well-known, but there is also a significant number of pathologic processes mediated by hormones, growth factors, cytosines and other inflammatory molecules whose action on the cardiomyocyte and the rest of the cellular and non-cellular components of the myocardium in a hypertensive patient which can explain the development of left ventricular hypertrophy and myocardial remodeling [4].
Likewise, an adequate treatment in the hypertensive patient can prevent the damage to target organs, [1,5,6-8], however; the control of HTN not always avoids these lesions. These facts mean that the presence of a group of factors increase the risk of hypertensive cardiopathy and are independent of the control of HTN [5,9-12].
Therefore, despite the existence of studies about cardiovascular risk factors and the important contribution they have to learn about this topic, it is necessary to continue its study for the high incidence and prevalence of hypertensive cardiopathy, which increases mortality and incapacity by cardiovascular diseases (CVD) in developed countries and in developing countries like Cuba.
For that reason we aimed at designing and validating an index, based on risk factors, to predict the development of hypertensive cardiopathy in patients with a diagnosis of essential arterial hypertension.
Methodological Design
A cohort prospective study was carried out in hypertensive patients assisted at the specialized arterial hypertension physicians’ office of the “Carlos Manuel de Céspedes” Specialty Policlinic attached to the General University Hospital, Bayamo Municipality, Granma Province, Cuba from January 1st, 2010 to December 31, 2016. The patients assisted had four appointments per year.
Inclusion and exclusion criteria
The study included hypertensive patients who were 18-year-old and older with a past personal history of essential HTN of five years or more, who did not have a diagnosis of hypertensive cardiopathy. The study excluded patients with ischemic cardiopathy, despite its high frequency in hypertensive patients, where the role of HTN, though evident, would not be the only important factor in its development (in the present study we evaluate the direct effects of HTN, so the inclusion of this condition would introduce selection and classification biases); for the same reason were excluded patients with interventricular and auriculoventricular conduction disorders and patients with valvular disease also have been excluded; in addition, it was taken into account that the patients did not suffer from other conditions which could cause cardiopathy such as myocardiopathies (in any of its clinical forms), diabetes mellitus, thyroid diseases, chronic renal failure, treatment with cytostatic drugs chronic inflammatory and collagen diseases. In the same way, patients with a diagnosis of hypertensive cardiopathy in the first follow-up year were excluded.
Patient source
The patients included in the cohort came from the hypertension physicians’ offices in each Health Area and were referred to the hospital Out-patient Department by the corresponding specialists. Every patient was submitted to detailed interview and physical examination to obtain the necessary data for the study. Later on, clinical evaluations were done every three months based on the analysis of the clinical data gathered; while echocardiogram and electrocardiogram were done every six months. When an excluding condition appeared, the patients were excluded from the study. Each individual evaluation concluded when the patient was diagnosed hypertensive cardiopathy or at the end of the study.
During the study all the patients received an initial uniform medical treatment based on the therapeutic protocol approved by the hospital Research Ethics Committee (according to the patient’s age, skin color, risk factors and contraindications. The protocol consisted, as a rule, in the use of an angiotensin II-converting enzyme inhibitor plus a diuretic; calcium channel blockers alone or combined with a diuretic; a beta-blocker alone or combined with a diuretic (according to the patient’s degree of HTN); and it was also kept in mind the latest recommendations about the treatment and management of HTN) to make as homogeneous as possible the factors which could have any influence on the evolution of the disease and were not considered direct object of study.
January 1, 2010 was defined as the zero hour or beginning of the cohort. Once the cohort had started it was decided not to include new patients (closed cohort). Every individual evaluation concluded when the patient developed hypertensive cardiopathy or after the seven-year period of the cohort for patients who did not develop the condition.
Sample characteristics
The cohort began with 1383 patients who were followed at the HTN physician’s office for seven years: n=937 patients came from urban areas (67.75%) and n=446 patients came from rural areas (32.25%) of our province. During the study 27 patients died of other causes than hypertensive cardiopathy and drop-outs for different reasons. Taking into consideration the criteria previously stated, 1255 patients were accepted; 429 (34.18%) of them developed hypertensive cardiopathy, out of which 248 (57.80%) were male patients.
Definition of variables
Dependent variable: onset of hypertensive cardiopathy, every hypertensive patient was diagnosed with this condition provided that in any of the follow-up appointments they began to meet the following criteria: LVH echocardiographic pattern: Dévereux’s formula was used [13]. (LV mass in grams)=0.8 (1.04 [left ventricular diastolic diameter+posterior wall thickness+interventricular septum thickness]3-[left ventricular diastolic diameter])3+0.6. Hypertrophy was considered at a value of ≥125 g/m2 in male and ≥110 g/m2 in female.
Diastolic dysfunction (DD) was considered (alteration in diastolic distensibility, filling or relaxation of the left ventricle: with slow LV relaxation and increased LV stiffness). Abnormal cut-off values: annular e velocity (septale_<7cm/s, and lateral e_<10cm/s), average E/e ratio>14; left atrium volume index>34 mL/m2, and peak tricuspid regurgitation (TR) velocity>2.8 m/s. LV DD is present if more thanhalf of the available parameters meet these criteria. Systolic dysfunction (ejection fraction<45%) by echocardiogram.
Clinical manifestations of cardiac failure of recent onset; [14] along with the echocardiographic findings previously described. Arrhythmia: persistent atrial fibrillation of long evolution and permanent fibrillation not caused by valve diseases, myocardiopathies, myocarditis, medications and drugs were considered. The diagnosis was based on the patient’s ambulatory clinical history, interview and physical exam. It was later confirmed by a standard twelve-lead electrocardiogram, according to the criteria proposed by the American Cardiology College and the American Heart Association [15].
Electrocardiograms were done by the physician’s office nurse using a portable digital electrocardiograph (CARDIOCID-BB, model A5102). Echocardiograms were done by two cardiologists with more than 15 years of experience and specialized in Echocardiography. An ASAOTE Caris PLUS machine was used following the American Echocardiography Association guidelines.
Independent variables
Included factors associated with the development of hypertensive cardiopathy that were being evaluated and are described below. Age was quantified in years. Patients over 60 years were considered exposed (dichotomic variable). Sex was divided into male and female. Smoking was grouped into two categories: (exposed) smokers if they smoked cigarettes, cigars, or pipe daily or almost daily, independent of the number of units smoked and ex-smokers, individuals who had quit the habit less than a year before, and non-smokers, those who had never been in the habit or who had quit it.
Alcoholism was considered in men who ingested more than an ounce of pure alcohol daily, equivalent to an ounce (20 ml) of ethanol, 8 ounces (240 ml) of wine, 24 ounces (720 ml) of beer, 1½ ounce (45ml) of rum and in the case of women and underweight patients those who consumed at least 15 ml per day [15].
Obesity was established by calculating body mass index (BMI greater or equal to 30: weight in kilograms/size in square meters) or a waist circumference greater or equal to 102 cm for men and 88 cm for women, or when both conditions were present. Sedentariness: subjects were considered sedentary if they spent daily less than a given amount of time in leisure activities that consume 4 or more metabolic equivalents (physical activity equivalent to or greater than (in energy output) to have a brisk walk (more than 6 km/h) or ride a bicycle at a speed between 16‐19 km/h). The patient’s profession was also taken into account. For the definition of the variable, the patients were asked the questions below, based on the data obtained from studies that related sedentariness and cardiovascular diseases [12,13]:
1. What kind of job do you do?
a) A job that involves little or no physical activity: usually sits down or stands up all day long or walks very little.
b) A job that demands a high energy output from the patient (example: construction workers, farmers, stevedores, etc.).
c) What kind of physical activity do you do in your free time?
Possible answers:
a) I never exercise.
b) Some physical or sports activity (at least 25 minutes for women and 30 for men) several times a month.
c) Regular physical activity (at least 25 minutes for women and 30 for men) several times a week.
d) Daily physical training.
Patients who answered affirmatively items 1 and 2 were considered sedentary. The rest of them were considered non-sedentary. Excessive sodium in the diet. Every subject who had an ingestion of salt greater than 5 grams per day (this is equivalent to more than a level teaspoonful, distributed among the dishes prepared for lunch and dinner) was considered exposed. As exposed were also included those patients who consumed bakery products or used table salt (three or more times a week) [16-19]. To obtain more accurate answers, the questions asked about consumed food, according to amount and frequency, the amount of sodium in the foods most frequently consumed, the amount of salt added while cooking and at the table, and the ingestion of foods with high sodium content; to obtain this information the following questions were used:
1. Do you (or anybody else at home) add more than a level teaspoonful of salt per person when cooking, distributed among the dishes prepared for lunch and dinner?
Possible answers:
a) Yes
b) No
2. Do you add salt to your food after it is cooked or do you use table salt shakers?
Possible answers:
a) Yes, every day or almost every day
b) Occasionally (less than three times a week)
c) Never
3. Do you eat salty foods? Such as: preserved foods and sausages (bacon, ham, sardines, olives, canned meat, salami, hot dogs, spiced sausage, and the like); foods that contain salt (crackers, bread, corn flakes, peanut, among others, sauces and canned soups, cheese, butter, mayonnaise, foods preserved in salt); other processed foodstuffs (bottled or carbonated soft drinks, beers, pickles, artificial flavors) or other salty foods (soy sauce, fish sauce, tomato sauce, sauces for local dishes)?
Possible answers:
a) Yes, every day or almost every day
b) Occasionally (less than three times a week)
c) Never
Patients who answered affirmatively any of the items 1a,2a or 3a were considered to have an excessive sodium intake in the diet (exposed).
The biomarkers selected as possible risk factors were cholesterol, uric acid, triglycerides, HDL-cholesterol, glycemia, C-reactive protein (CRP), microalbuminuria and the cholesterol/HDL quotient. Blood samples for laboratory tests were obtained in the fasting state (8 to 12 hours), and they were centrifuged at room temperature at 2000 rpm for 10 minutes. Creatinine, uric acid, cholesterol, HDL-cholesterol, triglycerides, and glycemia were measured with a HITACHI 902® machine during the first 24 hours after extraction and the first two ones were expressed in µmol/l and the rest in mmol/l. Determination of all the studies was done by means of enzymatic methods.
The cutpoints for the values of each quantitative variable were established according to the statistical estimates calculated. Variables were categorized trying to obtain the greatest statistical association and applicability of the results. To carry out this conversion the optimal cutpoint procedure was used. As optimal cutpoint was selected the value of C, for which the highest chi-square was obtained (or what is the same, the lowest value of the probability test) for all the values of the variable X that were categorized. In this way was selected the value that best differentiates the patients, according to the chi-square test association.
As cutpoints for the analysis were considered the following values: serum cholesterol (hypercholesterolemia) over 4.8 mmol/l, triglycerides (hypertriglyceridemia) greater than 1.7 mmol/l, HDL-cholesterol less than 1.5 mmol/l, cholesterol/HDL quotient higher than 4. The cutpoint for glycemia was established when the figures in fasting state reached values greater than 5.4 mmol/l, greater than 80 µmol/l for creatinine, and greater than 375 µmol/l for uric acid.
Non-ultrasensitive CRP was determined by the turbidimetric quantitative determination method and values over 4 mg/l were considered a potential risk factor.
Microalbuminuria patients were considered exposed when their values ranged from 0.02 to 0.2 g/l in a 24-hour period [6], and it was quantified by means of the Microalb-Latex technique (measurement of the amount of this substance in morning first-void urine specimen). Negative: suspension that stays homogeneous for the time the technique lasts [3 minutes]. Positive: presence of agglutination during the analysis indicates that albumin is present in the original sample).
The value of the quantitative variables was based on the average of three results in the first three appointments during the first year after the inclusion of the patient in the study. As controlled patients were defined those whose arterial blood pressure readings were lower than 140/90 mmHg (systolic and diastolic respectively) in the 100% of the determinations ( here were also included other determinations in different contacts with the health system for any reason; the patients had been instructed previously to bring their blood pressure readings, written by the corresponding practitioner in charge) during each follow-up year (at least four determinations per year) under medical treatment and not controlled those who did not meet the previous criteria. [16,20] To guarantee the authenticity of this variable, every patient was given a form that collected the following information: date, time, BP readings, and doctor’s signature and seal. Finally, the time of evolution and the HTN stage was considered. In the first case patients were grouped into two categories: patients with time of evolution between 5 and 15 years, and patients with time of evolution greater than 15 years. HTN stage was classified according to the Joint National Committee Seventh Report proposal and the measures proposed for the correct classification and determination of arterial blood pressure were also observed [1].
For the arterial blood pressure determinations were used aneroid and mercury sphygmomanometers previously calibrated by the Normalization and Quality Territorial Office, accredited for this purposes. Data were obtained in the doctor’s offices during the different interviews carried out by the authors with the patients’ informed consent.
Statistical analysis
The statistical analysis started with the characterization of the sample and the description of all the variables. The means, the medians (due to the presence of several variables with extreme values), and the standard deviations were determined for the quantitative variables, along with the minimum and maximum values of each distribution. Pearson’s chi-square test was calculated for the qualitative variables (Independence test) and Student's t test for the quantitative variables when variable distribution was acceptably similar either to the normal one or to Mann Whitney’s U; when the distribution differed from the normal; the significance level was also determined for each of them.
Index construction
It was thought that the index should contain items which could form a global index that would take the shape of a lineal combination between items: I=W1X1+W2X2+……+ WKXK. Where Xi is the i-th variable determined as a risk factor in each statistical analysis and Wi is the “weight” chosen for each variable. So, the construction phase was based on the selection of items that would shape the indicator and the search for the ponderations that should take each item in the lineal combination.
The index derived from Cox’s proportional regression analysis (a cohort previously done in the same population where the sample had been obtained ten years before) [21] and the cutpoints were selected on the condition that they were the ones that made the greatest contribution to the model and at the same time were significant from the clinical point of view. Each variable retained by the model was assigned a score using the hazard rate (HR) test and it was approximated to whole numbers. Then, the risk was classified in an ordinal scale, by dividing the index distribution into four zones framed by percentiles 10,50 and 90. In this way was achieved the risk index proposal, which can be classified as an ordinal variable with four categories from low to very high risk (category I {low}: 0 to 2 scores; category II {moderate}: 3 to 6 scores; category III {high}: 7 a 13 scores; category IV {very high}: 14 to 18 scores).
Internal validation of the index
Once the index was constructed, its predictive capacity was calculated: sensitivity, specificity, false positive rate (1- Specificity), positive predictive value, negative predictive value, positive and negative probability coefficient and the general e y la precision of the test. Youden’s index was also determined to evaluate the optimal cutpoint (allowed to classify its capacity: sensitivity+specificity–1).
External validation of the index
Content, presentation, construction and criterion validity were evaluated
Content and presentation validity
Expert consultation. Out of 29 possible experts examined were selected 10, by the preference qualimetric method, based on the determination of the expert’s competence and readiness to cooperate with our study. Self-evaluation of the study was used by the expert himself based on K coefficient, to obtain scores between 0.7 and 1.
K coefficient calculation: K=½ (Kc+ka) for 29 possible experts.
Where:
Kc: expert’s knowledge or information coefficient about the risk factors of hypertensive cardiopathy, calculated on the expert’s self-evaluation on a scale from 0 (total ignorance) to 10 (maximum knowledge) multiplied by 0.1.
Ka: argumentation coefficient of the criteria determined as result of the sum of the points achieved from a pattern table.
Calculations were done for each case and the argumentation coefficient was obtained for each expert, then the 10 with the highest competence were chosen, all of their scores ranged from 0.7 to 1, which meant that their competence level was average or high. The remaining 19 experts were excluded because their competence level was lower than 0.5. Each expert was consulted individually and in an anonymous way by means of guide elaborated for that purpose. Out of the 10 expert used, five were first and second degree specialists in Internal Medicine, PhDs in Medical Sciences and Full Professors, with more than 15 years of clinical, teaching and research experience. Five of these experts were specialists in Cardiology and had a PhD degree.
These experts were consulted anonymously, based on their knowledge and experience about HTN. The experts gave their opinion about the way in which the five basic conditions which should characterize an index were met. Each expert received a form for the recollection of information, the instructive document for its filling and a written explanation of the meaning of the aspects to be evaluated by them. The experts gave their opinion about the degree in which each of the elements was accomplished according to three possibilities: nothing, moderately or very much. The aspects to evaluate were: reasonable and comprehensible, sensitive to variations of the phenomenon measured, with justifiable basic suppositions, components clearly defined and whether they can be derived from obtainable data [22].
Construction validity
To evaluate this aspect it was taken into account that the greater morbidity corresponded to the patients classified in the categories of greater risk. The association between the ordinal index and the risk of hypertensive cardiopathy was evaluated based on the calculation of the association coefficient for ordinal and nominal variables, Eta. The index average values among the patients with hypertensive cardiopathy and without it were determined by Student’s t test for independent samples.
Criterion validity
It was evaluated the correlation between the index with four categories and an indicator of cardiovascular risk, the Framingham’s index [23], (this is a quantitative index, so it was divided into categories, as it was done with the scales of the present study) to calculate the possible association with the proposed indexes, using Kendall’s Tau-b association coefficient and chi-square tests. To evaluate the lineal association between the quantitative index and Framingham’s index [23], with the risk of hypertensive cardiopathy Pearson’s correlation coefficient was used.
The index discrimination capacity was determined by means of the analysis of the data generated by the ROC curves. Calibration was also estimated using the Hosmer and Lemeshow’s test, with a contrast in 10 cutpoints between the observed and expected results. A test result greater than 0,05 indicates a good calibration (Figure 1).
Reliability
Equivalence was demonstrated by means of ten doctors who played the role of “judges” and applied independently the instrument to sample validation forms. To evaluate concordance among the “judges” the correlation coefficients for all the possible pairs of judges were obtained. For the ordinal index, ponderated Kappa’s coefficient for more than two judges and the Kappa for each level were determined. To determine the statistical significance the global Kappa and the Kappa for each of them by category were calculated. Cronbach’s alpha and general and standardized alpha coefficients were used for the evaluation of internal consistence. All the statistical calculations were done with Windows SPSS software (version 22.0).
Ethical regulations
For the development of this study all the basic ethical regulations established for the research process in clinical and epidemiological studies were followed and the consent of the hospital Board of Directors and Ethics Committee was granted.
Bias control
With the aim of achieving the maximum accuracy and exactness of the necessary data for the study, selection, classification and information biases were taken into account.
Results
The index validation process was done with a sample of 1255 patients during a seven-year cohort. The average age was 58.63 (standard deviation: 12.08); while the biological marker with greatest standard deviation (99.81) was uric acid (mean: 344.28). The patients’ baseline characteristics are shown in table 1. It can be seen that there were significant differences in all the variables between the patients who developed hypertensive cardiopathy and those who did not.
| Table 1: Baseline characteristics of the study population. | ||||
| Variables | Hypertensive cardiopathy N=429 | Without ypertensive cardiopathy N=826 | Total N=55 | *p |
| C reactive protein>4mg/L | 345 | 289 | 634 | 0.000 |
| Age over 60 years | 344 | 279 | 623 | 0.000 |
| Time of evolution greater than 15 years | 322 | 316 | 638 | 0.000 |
| Creatinine≥80 µmol/L | 277 | 266 | 543 | 0.000 |
| No control of arterial hypertension | 277 | 229 | 506 | 0.000 |
| Stage 2 arterial hypertension | 274 | 236 | 510 | 0.000 |
| Microalbuminuria | 257 | 190 | 447 | 0.000 |
| HDL≤1.5 mmol/L | 256 | 232 | 488 | 0.000 |
| Smoking | 244 | 293 | 537 | 0.000 |
| Cholesterol≥4.8mmol/L | 240 | 169 | 409 | 0.000 |
| Excessive sodium in the diet | 230 | 287 | 517 | 0.000 |
| Uric acid ≥375 µmol/L | 207 | 180 | 387 | 0.000 |
| Cholesterol quotient/HDL≥4 | 222 | 134 | 356 | 0.000 |
| Glycemia≥5.4mmol/L | 196 | 84 | 280 | 0.000 |
| *p = 0.000 indicates<0.001. | ||||
Index construction
The index construction was done by means of a selection process of variables and their punctuation, based on the results obtained with Cox’s regression (data published in Mewade journal) [21] using the HR value. Table 2 shows the index with its items and ponderations. It also represents the four risk categories, with a high morbidity of categories III and IV. This fact should be emphasized since it implies that the index classifies correctly the patients with greater risk. As can be seen in table 3, the average values of the proposed index were significantly greater in patients with hypertensive cardiopathy (11.254; p=0.000) than in those who did not develop the condition; similar results were obtained with Framingham’ index.
Table 2: Quantitative and ordinal index proposed to predict the development of hypertensive cardiopathy. |
||
| Items | Ponderation | |
| Present | Absent | |
| No control of arterial hypertension | 2 | 0 |
| Stage 2 arterial hypertension | 2 | 0 |
| Microalbuminuria | 2 | 0 |
| Age over 60 years | 2 | 0 |
| Time of evolution of hypertension | 1 | 0 |
| Cholesterol | 1 | 0 |
| C reactive protein | 1 | 0 |
| HDL cholesterol (high density lipoprotein) | 1 | 0 |
| Smoking | 1 | 0 |
| Glycemia | 1 | 0 |
| Excessive sodium in the diet | 1 | 0 |
| Cholesterol quotient/HDL | 1 | 0 |
| Creatinine | 1 | 0 |
| Uric acid | 1 | 0 |
| Total | 18 | 0 |
| Risk Categories | Patients | Morbility |
| Category I: low risk (0-2 points) | 83 | 0 |
| Category II: moderate risk (3-6 points) | 468 | 2.56% |
| Category III: high risk (7-13 points) | 576 | 50.86% |
| Category IV: very high risk (14-18 points) | 128 | 96.87% |
| Total number of patients | 1255 | 34.18% |
| Table 3: Comparison of average values of the indexes being validated. | ||||||
| Indexes | Number | Mean | Standard deviation | t* | p† | |
| Proposed | Hypertensive Yes Cardiopathy No |
429 826 |
11.254 5.566 |
2.256 2.554 |
38.89 | 0.000 |
| Framingham | Hypertensive Yes Cardiopathy No |
429 826 |
4.960 2.714 |
1.639 1.544 |
23.92 | 0.000 |
| *Student's t test. †Student’s t test (p<0.0001). | ||||||
Internal validity of the index
The index sensitivity was of 97.20 (IC: 93, 93-94.09) and specificity of 65, 38 (IC: 76, 25-76, 20), and a validity index of 86, 50. The positive predictive value was 59, 32, while the negative value was 97.83. The positive verisimilitude rate was 2.81 and the negative of 0.04. Te optimar cutpoint waus 7 (Youden’s index of 0.62).
External validity
The index components were submitted to the consideration of experts for the analysis of presentation and content validity. It outstands that 90% considered that the content derived from obtainable data and the components were clearly defined. Construction validity was demonstrated with the value of Eta coefficient (0.660). 98% of the patients with hypertensive cardiopathy were classified in categories III and IV. Criterion validity was demonstrated by the significant statistic relation between the categories of the proposed index and the categories of Framingham’s index. The association coefficient (Tau b) was of 0.681 Table 4. The proposed index in its purely quantitative way showed a lineal and statistically significant correlation (p: 0.000) with Framingham’s index, as shows the value of Pearson’s correlation coefficient (0.811).
| Indexes | Area | p | Asymptotic interval of confidence (95%) | |
| Inferior limit | Superior limit | |||
| Predictive index of hypertensive cardiopathy | 0.944 | 0.000 | 0.932 | 0.956 |
| Framingham index | 0.832 | 0.000 | 0.809 | 0.856 |
| Table 4: Relation between the proposed index and the Framingham index with the risk of developing hypertensive cardiopathy. | |||||||
| Hypertensive cardiopathy | Categories | Framingham index | Total | ||||
| 1.00 | 2.00 | 3.00 | 4.00 | ||||
| Yes | Proposed index | 2.00 | 7 | 5 | 0 | 0 | 12 |
| 3.00 | 4 | 65 | 149 | 75 | 293 | ||
| 4.00 | 0 | 0 | 26 | 98 | 124 | ||
| Total | 11 | 70 | 175 | 173 | 429 | ||
| No | Proposed index | 1.00 | 74 | 9 | 0 | 0 | 83 |
| 2.00 | 118 | 272 | 65 | 1 | 456 | ||
| 3.00 | 7 | 95 | 147 | 34 | 283 | ||
| 4.00 | 0 | 0 | 0 | 4 | 4 | ||
| Total | 199 | 376 | 212 | 39 | 826 | ||
| Total | Proposed index | 1.00 | 74 | 9 | 0 | 0 | 83 |
| 2.00 | 125 | 277 | 65 | 1 | 468 | ||
| 3.00 | 11 | 160 | 296 | 109 | 576 | ||
| 4.00 | 0 | 0 | 26 | 102 | 128 | ||
| Total | 210 | 446 | 387 | 212 | 1255 | ||
| Kendall Tau-b = 0.681; p = 0.000 | |||||||
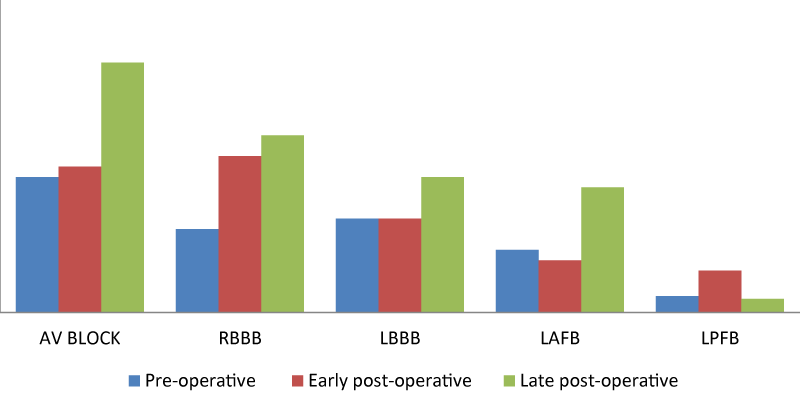
It can be seen in Graphic 1 that when the predictive capacity of the proposed index was compared with Framingham’s during the validation process, both had a good capacity to discriminate the patients who would develop hypertensive cardiopathy from those who would not, but the former had a better predictive value with an area under the ROC curve of 0,944. An adequate relation between the observed and expected cases in all risk levels are presented in table 5. Hosmer and Lemeshow’s test indicates a good calibration (p: 0.751). The value of the reliability coefficient (R), showed that most of the index variation was significantly due to the patients (R= 0.821; p=0.000). The correlation coefficients for all the pairs of observers were of 0.949 (p: 0.000) or higher. Concordance was demonstrated in the ten couples of “judges,” for all the categories (all greater tan 0), the global kappa coefficient was 0.983 (p<0.001).
| Table 5: Comparison between observed and expected morbidity in the index. Calibration. | |||||
| Steps | Without hypertensive cardiopathy | Hypertensive cardiopathy | Total | ||
| Observed | Expected | Observed | Expected | ||
| 1 | 124 | 124.717 | 4 | 3.283 | 4 |
| 2 | 78 | 78.237 | 8 | 7.763 | 8 |
| 3 | 79 | 76.975 | 16 | 18.025 | 16 |
| 4 | 59 | 60.542 | 35 | 33.458 | 35 |
| 5 | 43 | 40.794 | 51 | 53.206 | 51 |
| 6 | 24 | 22.805 | 69 | 70.195 | 69 |
| 7 | 10 | 13.794 | 104 | 100.206 | 104 |
| 8 | 6 | 6.614 | 114 | 113.386 | 114 |
| 9 | 5 | 2.532 | 100 | 102.468 | 100 |
| 10 | 1 | 1.988 | 325 | 324.012 | 325 |
Hosmer and Lemeshow Test X2 = 5.059 degrees of freedom 8 p = 0.0751. |
|||||
Cronbach’s alpha coefficient to evaluate the internal consistence was adequate (0.718, Table 6). As can be seen, no item had values lower tan 0.35; demonstrating an adequate internal consistency.
| Table 6: Elements of internal consistency of the proposed index. | |||
| Ítems | Ítem-total correlation (corrected) |
Determination coefficient | Alpha after removing the variable |
| No control of hypertension | 0.54 | 0.65 | 0.67 |
| HDL | 0.47 | 0.58 | 0.69 |
| Cholesterol coefficient /HDL | 0.46 | 0.55 | 0.69 |
| Age over 60 years | 0.45 | 0.34 | 0.71 |
| Cholesterol | 0.42 | 0.35 | 0.71 |
| Smoking | 0.40 | 0.38 | 0.74 |
| C reactive protein | 0.39 | 0.30 | 0.75 |
| Stage 2 hypertension | 0.39 | 0.29 | 0.76 |
| Time of evolution of hypertension | 0.38 | 0.21 | 0.75 |
| Microalbuminuria | 0.37 | 0.28 | 0.76 |
| Creatinine | 0.37 | 0.19 | 0.76 |
| Uric acid | 0.36 | 0.15 | 0.77 |
| Excessive sodium in the diet | 0.36 | 0.11 | 0.77 |
| Glycemia | 0.35 | 0.08 | 0.78 |
| Cronbach’s alpha= 0.718 Alpha of standardized items 0.721. | |||
Discussion
Stratifying correctly cardiovascular risk in general and the risk of hypertensive cardiopathy in particular is a complex task. For the latter there is currently an index designed in our context, consisting on a multivariate study, based on a case-control study [24]. Although the study showed an adequate internal and external validity [24], it is necessary to improve it based on the fact that the risk of developing depends not only on multiple causes but also with permanent evolutional changes, as has been demonstrated by several studies [21,24-29]. Another aspect to highlight is that the new proposal is based on a cohort study, which have demonstrated a better capacity to predict risks. In the present study a solution is offered in this respect. An index was designed based on the results previously obtained in a multivariable analysis [21], which includes 14 items. An index based on a cohort has not been tried for hypertensive cardiopathy. In a study to estimate cardiovascular risk in a Cuban population, De la Noval García [30] found that the use of predictive tables of cardiovascular risk of the WHO/ISH, underestimates it in the population studied.
In a transversal study Armas Rojas [31], found that WHO/ISH cardiovascular risk tables classified most patients as low risk, in spite of the high prevalence of risk factors in the studied population. In order to evaluate global cardiovascular risk, a model with adequate discriminative capacity and calibration was constructed, but it has the limitation that it was validated in a predominantly foreign white population and it does not stratify risk by cardiovascular diseases in particular [32]. In this regard, it must be emphasized that although there are indexes to estimate total cardiovascular risk, it does not seem coherent to include hypertensive cardiopathy, since despite the fact that it shares several risk factors with the rest of the CVD, some of these conditions are cause of LVH, heart failure and conduction disorders (manifestations present in, just to avoid confusion). On the other hand, Ang [33] validates a clinical scale to identify LVH by echocardiogram; in the study few factors were considered, so its use can underestimate the risk in the Cuban population.
In order to solve this problem, an index was constructed and validated to predict the risk of developing that fits the context where the study was carried out and also that meets the morbidity probabilistic needs of vulnerable populations. The construction process evidenced that the proposed index can predict the development of hypertensive cardiopathy properly; it should be pointed out that the high negative predictive values indicate that it is improbable that the index classifies as low risk individuals who develop the disease. It was found, in addition, that the optimal cutpoint corresponds to the high risk category (III), an aspect to be kept in mind when using the index. To check presentation and content validity, the recommendations found in the literature were taken into account [22].
The result of this process was considered satisfactory. Construction validity was evidenced since it was demonstrated that in the highest risk categories are present in the majority of hypertensive cardiopathy patients; and criterion validity was demonstrated by comparing the index with a version of Framingham’s index. It should be stated that the proposed scale had greater discriminative capacity, probably because a larger number of variables was used, based on current physiopathological knowledge and new risk factors for hypertensive cardiopathy, [5,6,34,35] as well as the use of cutpoints with greater sensitivity and specificity of the biological variables, taking into account the characteristics of the population studied, without extrapolation from foreign studies, an aspect which does not limit the use of this index in other populations.
The correlation coefficients obtained from the concordance between the judges and the kappa were adequate according to the literature [36,37]. They revealed that with some advice the doctors who assist the hypertensive patients can use the index to predict the risk of hypertensive cardiopathy with a minimum error. The index had an adequate internal consistency, as it is shown by the value of Cronbach’s Alpha coefficient [38]. It can be seen that none of the items has values under 0, 35, which means that the use of each of them to predict the risk of hypertensive cardiopathy is adequate and measure what is really meant to be measured by means of them.
Conclusion
This study proposes and index to predict the risk of developing hypertensive cardiopathy based on a multivariate analysis of risk factors (cohort previously published) with an appropriate internal validity. The index also exhibits an adequate capacity of discrimination and calibration (external validity). The instrument can be used for clinical and epidemiological surveillance, taking into account that it permits to identify the subjects with greater probability of developing the condition and stratify the risk.
Novelty and limitations
The novelty of this study consists in its originality and the fact that the quality of previous case and control studies published by these authors has been improved [24]. In addition, the present model isolates the evaluation of subjects and is concerned with only one cardiovascular event (hypertensive cardiopathy). Nevertheless, it has as major limitations the size of the sample and the fact that the application of the model in the care of hypertensive patients will depend on how appropriately it can be used by the doctors in charge of providing health care to those patients.
Acknowledgments
The authors acknowledge the valuable contribution of the Clinical Laboratory, Imaging and Cardiology Departments.
References
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 report. 2003; 289: 2560-2572. Ref.: https://goo.gl/s9MtBw
- República de Cuba. Anuario Estadístico de Salud; 2016. [citado 10 abril 2017]. Disponible en.
- Tientcheu D, Ayers C, Das SR, McGuire DK, de Lemos JA, et al. Target organ complications and cardiovascular events associated with masked hypertension and white-coat hypertension. Analysis from the Dallas heart study. Am Coll Cardiol. 2015; 66: 2159-2169. Ref.: https://goo.gl/B4sMN3
- Díez J, Frohlich E D. A translational approach to hypertensive heart disease. Hypertension. 2010; 55: 1-8. Ref.: https://goo.gl/xNGLyg
- Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, et al. Guía de práctica clínica de la ESH/ESC 2013 para el manejo de la hipertensión arterial. Rev Esp Cardiol. 2013; 66: 880.
- Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burniere M, et al. Reappraisal of European guidelines on hypertension management: A European Society of Hypertension Task Force document. J Hypertens. 2009; 27: 2121-2158. Ref.: https://goo.gl/HBrVk9
- Maione A, Annemans L, Strippoli G. Proteinuria and clinical outcomes in hypertensive patients. Am J Hypertens. 2009; 22: 1137-1147. Ref.: https://goo.gl/w2pMxY
- Angeli F, Ambrosio G. Mecanismos de la hipertrofia ventricular izquierda en la hipertensión: más que solo la presión arterial. Rev Argent Cardiol. 2015; 83: 6-7. Ref.: https://goo.gl/1BKVsC
- Harbaoui B, Courand PY, Defforges A, Khettab F, Milon H, et al. Cumulative effects of several target organ damages in risk assessment in hypertension. Am J Hypertens. 2016; 29: 234-244. Ref.: https://goo.gl/MFLhNw
- Wang SX, Xue H, Zou YB, Sun K, Fu CY, et al. Prevalence and risk factors for left ventricular hypertrophy and left ventricular geometric abnormality in the patients with hypertension among Han Chinese. Chin Med J. 2012; 125: 21-26. Ref.: https://goo.gl/SesKhT
- Sharman J E. New insights into cardiovascular risk from the exercise central waveform. Artery Res. 2009; 2: 132-137. Ref.: https://goo.gl/Zd9a6A
- García Iglesias A, Lozano Alonso J E, Álamo Sanz R, Vega Alonso T. Factores asociado al control de la presión arterial en la cohorte del estudio del riesgo de enfermedad cardiovascular en Castilla y León (RECCyL). Hipertens Riesgo Vasc. 2015; 32: 48-55. Ref.: https://goo.gl/AAKq4U
- Dévereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. 1977; 55: 613-618. Ref.: https://goo.gl/VwxWXY
- Khouri MG, Peshock RM, Ayers CR, de Lemos JA, Drazner MH. A 4-tiered classification of left ventricular hypertrophy based on left ventricular geometry: The Dallas Heart Study. Circ Cardiovasc Imaging. 2010; 3: 164-171. Ref.: https://goo.gl/8Fnptm
- Fuster V, Rydén L E, Cannom D S, Crijns H J, Curtis A B, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation. J Am Coll Cardiol. 2011; 123: 104-123. Ref.: https://goo.gl/uYTEgW
- Pérez Caballero MD, Dueñas Herrera A, Alfonso Guerra JP, Vázquez Vigoa A, Navarro Despaigne D, et al. Hipertensión arterial. Guía para la prevención, diagnóstico y tratamiento. Comisión Nacional Técnica Asesora del Programa de Hipertensión Arterial. La Habana: Editorial Ciencias Médicas. 2008. Ref.: https://goo.gl/d9zaUu
- Whelton S, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002; 136: 493-503. Ref.: https://goo.gl/FsyiuG
- Cabrera de León A, Rodríguez-Pérez C, Rodríguez-Benjumeda M, Anía-Lafuente B, Brito-Díaz B, et al. Sedentarismo: tiempo de ocio activo frente a porcentaje del gasto energético. Rev Esp Cardiol. 2007; 60: 244-250. Ref.: https://goo.gl/9V1PG6
- Zhao W, Hasegawa K, Chen J. Part A. Recent advances in dietary assessment tools. The use of food-frequency questionnaires for various purposes in China. Public Health Nutrition. 2002; 5, 829-833. Ref.: https://goo.gl/Romh5u
- Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010; 303: 2043-2050. Ref.: https://goo.gl/JHFMTu
- Álvarez Aliaga A, González Aguilera JC, Maceo Gómez LR. Factores asociados al desarrollo de la cardiopatía hipertensiva: un estudio de cohorte, en Bayamo, Cuba. Medwave. 2016; 16. Ref.: https://goo.gl/csGC8P
- Moriyama IM. Problems in the measurement of health status. En: Sheldon EB, Moore W. eds. Indicators of social change: concepts and measurements. New York: Rusell Sage fundation. 1968: 573-599.
- D'Agostino RB, Grundy S, Sullivan LM, Wilson P, for the CHD Risk Prediction Group. Validation of the Framingham Coronary Heart Disease Prediction Scores. Results of a multiple ethnic groups investigation. JAMA. 2001; 286:180-187. Ref.: https://goo.gl/UBzXFm
- Álvarez Aliaga A, González Aguilera JC, Quesada Vázquez AJ, Frómeta Guerra A, Cisneros Sánchez L, Maceo Gómez LR. Índice predictivo para la cardiopatía hipertensiva. Rev Cubana de Med. 2010; 49: 311-329. Ref.: https://goo.gl/2pBkEe
- Drazner M H. The Progression of Hypertensive Heart Disease. Circulation. 2011; 123: 327-334. Ref.: https://goo.gl/chYmgm
- Cuspidi C, Giudici V, Negri F, Meani S, Sala C, et al. Improving cardiovascular risk stratification in essential hypertensive patients by indexing left ventricular mass to height(2.7). J Hypertens. 2009; 27: 2465-2471. Ref.: https://goo.gl/Jvobsg
- Gu Q, Dillon CF, Burt VL, Gillum RF. Association of hypertension treatment and control with all-cause and cardiovascular disease mortality among US adults with hypertension. Am J Hypertens. 2010; 23: 38-45. Ref.: https://goo.gl/k3x92g
- Peralta CA, Katz R, Newman AB, Psaty BM, Odden MC. Systolic and diastolic blood pressure, incident cardiovascular events, and death in elderly persons: the role of functional limitation in the Cardiovascular Health Study. Hypertension.2014; 64: 472-480. https://goo.gl/d2GVgz
- Álvarez Aliaga A, González Aguilera JC. Algunos factores de riesgo de la cardiopatía hipertensiva. Rev Cubana de Med. 2009; 48: 139-151. Ref.: https://goo.gl/vSJHBL
- De la Noval García R, Armas Rojas NB, de la Noval González I, Fernández González Y, Pupo Rodríguez HB, et al. Estimación del riesgo cardiovascular global en una población del área de salud Mártires del Corynthia. Ciudad Habana, Cuba. Rev Cubana Cardiol Cir Cardiovasc. 2011; 17: 62-68. Ref.: https://goo.gl/77vWvG
- Armas Rojas NB, De la Noval García R, Dueñas Herrera A, Castillo Núñez JC, Suárez Medina R, et al. Estimación del riesgo cardiovascular mediante tablas de la Organización Mundial de la Salud. Área de salud “Héroes del Moncada”. 2011. Rev Cubana Cardiol Cir Cardiovasc. 2014; 20. Ref.: https://goo.gl/x1U0K2
- D’Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, et al. General cardiovascular risk profile for use in primary care the Framingham heart study. Circulation. 2008; 117: 743-753. Ref.: https://goo.gl/XgFgAh
- Ang DSC, Fahey TP, Wright GA, Struthers AD. Development and validation of a clinical score to identify echocardiographic left ventricular hypertrophy in patients with cardiovascular disease. Am J Hypertens.2008; 21: 1011-1017. Ref.: https://goo.gl/8VWSLa
- Creemers EE, Pinto YM. Molecular mechanisms that control interstitial fibrosis in the pressure-overloaded heart. Cardiovasc Res. 2011; 89: 265-272. Ref.: https://goo.gl/fJ85zY
- Drazner MH. The Progression of Hypertensive Heart Disease. Circulation. 2011; 123: 327-334. Ref.: https://goo.gl/chYmgm
- Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problem of two paradoxes. J Clin Epidemiol. 1990; 43: 543-549. Ref.: https://goo.gl/8NisKG
- Streiner DL, Norman GR. Health measurement scales. A practical guide to their development and use. Oxford: Oxford University Press; 1989: 144-161.
- García Cadena CH. La medición en las ciencias sociales y la psicología, en estadística con SPSS y metodología de la investigación de René Landeros Hernández y Mónica T González Ramírez. México, Trillas (comp). 2006. Ref.: https://goo.gl/RY1Qad