Abstract
Research Article
Ivabradine versus carvedilol in the management of palpitation with sinus tachycardia among recovered COVID-19 patients
Kartik Pandurang Jadhav* and Pankaj V Jariwala
Published: 23 December, 2020 | Volume 5 - Issue 3 | Pages: 176-180
Introduction: One of the major complications among COVID-19 patients include cardiac arrhythmias. Commonest arrhythmia is sinus tachycardia which is usually associated with palpitation causing discomfort to patients. In this study, we present a comparative study of use of Ivabradine vs. Carvedilol for sinus tachycardia in post-COVID-19 infected patients.
Method: 50 consecutive recovered COVID-19 patients with sinus tachycardia were included in this open labelled RCT. 25 patients received Ivabradine and remaining 25 received Carvedilol. Single therapy non-responders were treated with Ivabradine with Atorvastatin.
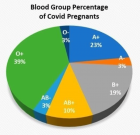
Results: The mean age of all patients is 48.8±7.66 years (Males 49.5 ± 7.21 years; Females 47.68 ± 8.23 years). The mean heart rate (MHR) of all patients is 125.52 ± 9.07/min (Males 125.67 ± 8.78/min; Females 125.26 ± 9.5/min). After five days of single drug therapy the mean drop in the heart rate was 35.04 ± 10.55/min (Males 34.41 ± 9.71/min; Females 36.05 ± 11.72/min), resulting in 27.88 ± 8.11% (Males 27.38 ± 7.56%; Females 28.69 ± 8.89%) reduction in MHR. Among the two groups, the Carvedilol group showed improvement of MHR in 14(56%) patients; whereas in Ivabradine group 18(72%) patients improved out of 25 patients each (p: 0.2385). In the Carvedilol group the MHR reduced from 128.6 ± 8.44 to 95.68 ± 10.63 (p < 0.001), which is statistically significant; similarly, the Ivabradine group showed a MHR from 122.44 ± 8.62 to 85.28 ± 10.52 (p < 0.001). The monotherapy therapy non-responders were treated with dual-therapy of (Ivabradine + Atorvastatin).
Discussion: Ivabradine is more effective in controlling heart rate compared to Carvedilol. Also, Ivabradine group scores very well in ‘patient-satisfaction’ with regards to symptom (palpitation) relief.
Conclusion: The COVID-19 sequelae of sinus tachycardia can be better controlled with Ivabradine when compared to Carvedilol.
Read Full Article HTML DOI: 10.29328/journal.jccm.1001107 Cite this Article Read Full Article PDF
Keywords:
COVID-19; Recovered COVID-19; Sinus tachycardia; Carvedilol in COVID-19; Ivabradine in COVID-19
References
- WHO Timeline - COVID-19. WHO official website. 2020. https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19
- Sharma S, Singh G. Prevalence and Global Impact of 2019-nCoV Zoonotic Viruses on China and World: Consequences of Chaotic and Stressed Environment. Int J Computer Applications. 2020; 12: 16.
- Sharma S, Sharma M, Singh G. A chaotic and stressed environment for 2019-nCoV suspected, infected and other people in India: Fear of mass destruction and causality. Asian J Psychiatr. 2020; 51: 102049. PubMed: https://pubmed.ncbi.nlm.nih.gov/32278890/
- Gautam R, Sharma M. 2019-nCoV pandemic: A disruptive and stressful atmosphere for Indian academic fraternity. Brain Behav Immun. 2020; 88: 948–949. PubMed: https://pubmed.ncbi.nlm.nih.gov/32289366/
- Wang D, Hu B, Hu C, Zhu F, Liu X, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA. 2020; 323: 1061-1069. PubMed: https://pubmed.ncbi.nlm.nih.gov/32031570/
- Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020; 5: 1265-1273. PubMed: https://pubmed.ncbi.nlm.nih.gov/32730619/
- Liu K, Fang YY, Deng Y, Liu W, Wang MF, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J. 2020; 133: 1025–1031. PubMed: https://pubmed.ncbi.nlm.nih.gov/32044814/
- Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, et al. Guidance for Cardiac Electrophysiology During the COVID-19 Pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Heart Rhythm. 2020; 17: e233-e241. PubMed: https://pubmed.ncbi.nlm.nih.gov/32247013/
- Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020; 41: 1798–1800. PubMed: https://pubmed.ncbi.nlm.nih.gov/32186331/
- Babapoor-Farrokhran S, Gill D, Walker J, Rasekhi RT, Bozorgnia B, et al. Myocardial injury and COVID-19: Possible mechanisms. Life Sci. 2020; 253: 117723. PubMed: https://pubmed.ncbi.nlm.nih.gov/32360126/
- Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C. Cardiac and arrhythmic complications in patients with COVID‐19. J Cardiovasc Electrophysiol. 2020; 31: 1003–1008. PubMed: https://pubmed.ncbi.nlm.nih.gov/32270559/
- Tse S, Mazzola N. Ivabradine (Corlanor) for Heart Failure: The First Selective and Specific I f Inhibitor. PT. 2015; 40: 810–814. PubMed: https://pubmed.ncbi.nlm.nih.gov/26681903/
- Totura AL, Whitmore A, Agnihothram S, Schäfer A, Katz MG, et al. Toll-Like Receptor 3 Signaling via TRIF Contributes to a Protective Innate Immune Response to Severe Acute Respiratory Syndrome Coronavirus Infection. MBio. 2015; 6: e00638-15. PubMed: https://pubmed.ncbi.nlm.nih.gov/26015500/
- Chen WR, Liu HB, Sha Y, Shi Y, Wang H, et al. Effects of Statin on Arrhythmia and Heart Rate Variability in Healthy Persons With 48‐Hour Sleep Deprivation. J Am Heart Assoc. 2016; 5: e003833. PubMed: https://pubmed.ncbi.nlm.nih.gov/27799236/
- Kow CS, Hasan SS. Meta-analysis of Effect of Statins in Patients with COVID-19. Am J Cardiol. 2020; 134: 153–155. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7419280/
Figures:
Figure 1

Figure 2
Similar Articles
-
Ivabradine versus carvedilol in the management of palpitation with sinus tachycardia among recovered COVID-19 patientsKartik Pandurang Jadhav*,Pankaj V Jariwala. Ivabradine versus carvedilol in the management of palpitation with sinus tachycardia among recovered COVID-19 patients. . 2020 doi: 10.29328/journal.jccm.1001107; 5: 176-180
-
Association Between Electrocardiographic Abnormalities and In-Hospital Adverse Outcome in COVID-19 PatientsAnjuman Begum*, Wadud Chowdhury, Suman KS, Arnab KC, Md. Akteruzzaman, Barua Sushanta. Association Between Electrocardiographic Abnormalities and In-Hospital Adverse Outcome in COVID-19 Patients. . 2024 doi: 10.29328/journal.jccm.1001196; 9: 148-152
Recently Viewed
-
Psychosis in Parkinson’s Disease and Current Management Trends- an Updated Review of LiteratureRajib Dutta*. Psychosis in Parkinson’s Disease and Current Management Trends- an Updated Review of Literature. J Neurosci Neurol Disord. 2023: doi: 10.29328/journal.jnnd.1001078; 7: 027057
-
Enhancing adipose stem cell chondrogenesis: A study on the roles of dexamethasone, transforming growth factor β3 and ascorbate supplements and their combinationBernard J Van Wie*,Arshan Nazempour##,Chrystal R Quisenberry##,Nehal I Abu-Lail. Enhancing adipose stem cell chondrogenesis: A study on the roles of dexamethasone, transforming growth factor β3 and ascorbate supplements and their combination. J Stem Cell Ther Transplant. 2017: doi: 10.29328/journal.jsctt.1001004; 1: 028-051
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Response of Chemical Fertilisation on Six-year-old Oil Palm Production in Shambillo-Padre Abad- UcayaliEfraín David Esteban Nolberto, Guillermo Gomer Cotrina Cabello*, Robert Rafael-Rutte, Jorge Luis Bringas Salvador, Mag. Carmen Luisa Aquije Dapozzo, Guillermo Vilchez Ochoa, Luis Alfredo Zúñiga Fiestas, Nancy Ochoa Sotomayor, Mg. Merici Medina Guerre. Response of Chemical Fertilisation on Six-year-old Oil Palm Production in Shambillo-Padre Abad- Ucayali. Arch Food Nutr Sci. 2024: doi: 10.29328/journal.afns.1001058; 8: 024-028
-
Forensic analysis of private browsing mechanisms: Tracing internet activitiesHasan Fayyad-Kazan*,Sondos Kassem-Moussa,Hussin J Hejase,Ale J Hejase. Forensic analysis of private browsing mechanisms: Tracing internet activities. J Forensic Sci Res. 2021: doi: 10.29328/journal.jfsr.1001022; 5: 012-019
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."