Abstract
Research Article
Long-term results for post-interventional systemic heparinization following angioplasty of peripheral vessels
Masoud Mirzaie*, Zaur Guliyev and Mohammed Dakna
Published: 15 June, 2020 | Volume 5 - Issue 2 | Pages: 121-130
Objective: The long-term outcome of percutaneous transluminal angioplasties is mainly determined by restenoses, either by progression of the underlying disease or by intimal hyperplasia. Pharmacological substances on the one hand and the implantation of stents on the other have been developed with the intention of preventing precisely this complication. While patients are treated after PTA of peripheral vessels with different low-molecular-weight heparins, the indication for stent implantation is determined individually rather by experience. The aim of this study was to determine gender-specific risk factors of long-term outcome after percutaneous transluminal angioplasty (PTA) of peripheral vessels with or without stentimplantation.
Methods: In the present study, we examined the long-term results of percutaneous transluminal angioplasty (PTA) of peripheral vessels. Between 2007 and 2017, in total, 3,276 patients underwent PTA with or without stent implantation in our clinic. All patients were treated postinterventionally for 48 hours with 25,000 IU heparin (Unfractionated Heparin (UFH), heparinsodium-Braun, 25,000 I.E./5 ml, 2 ml/h) monitored by the partial thromboplastin time and subsequently underwent a control investigation every 6 months. The endpoint of the study was determination of symptomatic stenosis larger than 50% that required reintervention.
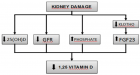
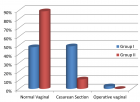
Results: 239 (68.2% with mean age 68.02 years) male patients and 111 female patients (31.71% with mean age 62.92 years) were evaluated with complete follow-up. A total of 470 PTAs were performed on male patients and 213 on female patients in multiple interventions. The majority of patients at the time of treatment were in stage IIb according to the classification of Fontaine (81.6% of male patients and 68% of females). In our sample, peripheral arterial disease stage III and IV according to Fontaine classification occurred twice as frequently in female patients as in male patients (stage III in 12.6% in female versus 6.1% in male, and stage IV in 18% in female versus 8.9% in males). In both groups, the femoral superficialis artery was most frequently dilated (64 cases, 30% in female and 155 cases, 32.9% in male), followed by the iliacal communis artery (46 cases in female and 99 cases in male, both with 21.5%). A balloon angioplasty of the tibialis anterior and posterior arteries was performed twice as frequently in female patients as in male patients (28 cases with 13.1% of tibialis ant. artery in female versus 32 cases with 6.8% in male patients, and in 17 cases with 7.9% of tibialis post. artery in female versus 16 cases with 3.4% in male patients). In this study, without consideration of gender, patency rates of 79% after 2.5 years, 67% after 5 years, 49% after 7.5 years and 37% after 10 years were determined for PTA without stent implantation. Between the 7th and 10th year in follow-up, the cumulative patency rates for stent implantation was 49%, whereas it was 31% for PTA alone. The results of this study show that the stent assisted PTA`s of comm. artery and external iliacal artery are significantly independent of risk factors better than the femoral vessels, and these in female patients better than in male patients. Male patients do not benefit significantly from stent implantation in the long term. As the COXI and II regression analyses show, gender-linked results are most evident for renal insufficiency and diabetes mellitus, and less pronounced also for the number of open lower leg vessels.
Conclusion: Under consideration of gender and risk factors, while male patients with diabetes mellitus, renal insufficiency and/or poor run-off did not benefit from stent implantation in the long-term, female patients with similar risk factors showed higher patency rates after stent therapy. In addition, the long-term results after PTA of femoral superficialis artery and poplitea artery are significantly worse than PTA of the pelvic vessels in both genders.
Read Full Article HTML DOI: 10.29328/journal.jccm.1001098 Cite this Article Read Full Article PDF
References
- Tendera M, Aboyans V, Bartelink ML, Baumgartner I, Clément D, et al. ESC Committee for Practice Guidelines: ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2011; 32: 2851–2906. PubMed: https://pubmed.ncbi.nlm.nih.gov/21873417/
- Tsetis D, Belli AM. Guidelines for stenting in infrainguinal arterial disease. Cardiovasc Intervent Radiol. 2004; 27: 198–203. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15129334
- Gur I, Lee W, Akopian G, Rowe VL, Weaver FA, et al. Clinical outcomes and implications of failed infrainguinal endovascular stents. J Vasc Surg. 2011; 53: 658–666. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21257284
- Armstrong EJ, Saeed H, Alvandi B, Singh S, Singh GD, Yeo KK et al. Nitinol self-expanding stents vs. balloon angioplasty for very long femoropopliteal lesions. J Endovasc Ther. 2014; 21: 34–43. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24502482
- Cassese S, Byrne RA, Ott I, Ndrepepa G, Nerad M, et al. Paclitaxel-coated versus uncoated balloon angioplasty reduces target lesion revascularization in patients with femoropopliteal arterial disease: a meta-analysis of randomized trials, Circ Cardiovasc Interv, 2012; 5: 582–589. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22851526
- Dake MD, Ansel GM, Jaff MR, Ohki T, Saxon RR, et al. Paclitaxeleluting stents show superiority to balloon angioplasty and bare metal stents in femoropopliteal disease: twelve-month Zilver PTX randomized study results. Circ Cardiovasc Interv. 2011; 4: 495–504. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21953370
- Duda SH, Pusich B, Richter G, Landwehr P, Oliva VL, et al. Sirolimus-eluting stents for the treatment of obstructive superficial femoral artery disease: six-month results. Circulation. 2002; 106: 1505–1509. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12234956
- Saxon RR, Dake MD, Volgelzang RL, Katzen BT, Becker GJ. Randomized, multicenter study comparing expanded polytetrafluoroethylene-covered endoprosthesis placement with percutaneous transluminal angioplasty in the treatment of superficial femoral artery occlusive disease. J Vasc Interv Radiol. 2008; 19: 823–832. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18503895
- Schillinger M, Schila Sabeti S, Loewe C, Dick P, Amighi J, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006; 354: 1879–1888. PubMed: https://pubmed.ncbi.nlm.nih.gov/16672699
- Sabeti S, Schillinger M, Amighi J, Sherif C, Mlekusch W, et al. Primary patency of femoropopliteal arteries treated with nitinol versus stainless steel self-expanding stents: propensity score-adjusted analysis. Radiology. 2004; 232: 516-521. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15286322
- Laird JR, Katzen BT, Scheinert D, Lammer J, Carpenter J, et al. Nitinol stent implantation versus balloon angioplasty for lesions in the superficial femoral artery and proximal popliteal artery: twelve-month results from the RESILIENT randomized trial. Circ Cardiovasc Interv. 2010; 3: 267–276. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22313193
- Chan AW. Clinical Evaluation of Restenosis. In: FUSTER, Valentin (Hrsg.): Topol EJ. (Hrsg.): Nabel E (Hrsg.): Atherothrombosis and coronary artery disease. 2. Edition, Philadelphia. Lippincott Williams & Wilkins, 2004.
- Franco CD, Hou G, Bendeck MP. Collagens, Integrins, and the Discoidin Receptors in Arterial Occlusive Disease. Trends Cardiovasc Med. 2002; 12: 143-148. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12069752
- Kim MS, Dean LS. In-Stent Restenosis: Cardiovasc Therapeutics. 2011; 29: 190-198. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20406239
- Dotter CT, Judkins MP. Transluminal treatment of arteriosclerotic obstruction Description of a new technique and preliminary report of its application. Circulation. 1964; 30: 654-670. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/14226164
- Shammas NW, Lemke JH, Dippel EJ, McKinney DE, Takes VS, et al. Bivalirudin in peripheral vascular interventions: a single center experience, 2003. J Invasive Cardiol. 2003; 15: 401-404. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12840239
- Shammas NW, Lemke JH, Dippel EJ, McKinney DE, Takes VS, et al. In-hospital complications of peripheral vascular interventions using unfractionated heparin as the primary anticoagulant. J Invasive Cardiol. 2003; 15: 242-246. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12730630
- Shammas NW. An overview of antithrombins in peripheral vascular interventions. J Invasive Cardiol. 2004; 16: 440-443.
- Valgimigli M, Gargiulo G. Activated Clotting Time During Unfractionated Heparin-Supported Coronary Intervention. JACC. 2018; 11: 1046-1049. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29778730
- Kimura T, Takeshi M, Ken K, Yasuhiro H, Teruyoshi K, et al. Comparisons of Baseline Demographics, Clinical Presentation, and Long-Term Outcome Among Patients With Early, Late, and Very Late Stent Thrombosis of Sirolimus-Eluting Stents. Circulation. 2010; 122: 52-61. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20566955
- Sudhir R, Yoshihisa K, Mitsuyasu T, Osamu K, Hitoshi M, et al. A comparison of clinical presentations, angiographic patterns and outcomes of in-stent restenosis between bare metal stents and drug eluting stents. EuroIntervention. 2010; 5: 841-846. PubMed: https://pubmed.ncbi.nlm.nih.gov/20142201
- Grimfjärd P, James S, Persson J, Angerås O, Koul S, et al. Outcome of percutaneous coronary intervention with the Absorb bioresorbable scaffold: data from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). EuroIntervention. 2017; 13: 1303-1310. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28781242
- Alshehri AM, Azoz AM, Shaheen HA, Farrag YA, Aldeen A, et al. Acute effects of cigarette smoking on the cardiac diastolic functions. J Saudi Heart Assoc. 2013; 25: 173–179. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24174857
- McGill HC. The cardiovascular pathology of smoking. Am Heart J. 1988; 115: 250-257. PubMed: https://pubmed.ncbi.nlm.nih.gov/3276113
- Bullen C. Impact of Tobacco Smoking and Smoking Cessation on Cardiovascular Risk and Disease. Expert Review of Cardiovascular Therapy. 2008; 6: 883-895. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18570625
- Khalilzadeh O, Baerlocher M, Shyn B, Connolly B, Devane A, et al. Proposal of a New Adverse Event Classification by the Society of Interventional Radiology Standards of Practice Committee. J Vasc Int Radiol, 2017; 28: 1432-1437. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28757285
- Tesdal I, Krzemien C, Weiß C. Balloon angioplasty of the crural arteries: angiographic and clinical long-term follow-up. JVIR. 2016; 27: 71–72.
- Ai H, Wang X, Suo M, Liu JC, Wang CG, et al. Acute- and Long-term Outcomes of Rotational Atherectomy followed by Cutting Balloon versus Plain Balloon before Drug-Eluting Stent Implantation for Calcified Coronary Lesions.Chin Med J (Engl). 2018; 131: 2025-2031. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30127211
- Kufner S, Joner M, Thannheimer A, Hoppmann P, Ibrahim T, et al. ISAR-TEST 4 (Intracoronary Stenting and Angiographic Results: Test Efficacy of 3 Limus-Eluting Stents) Investigators. Circulation. 2019; 139: 325-333. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30586724
- Borhani S, Hassanajili S, Tafti SHA, Rabbani S. Cardiovascular stents: overview, evolution, and next generation. Prog Biomater. 2018; 7: 175–205. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30203125
- Janas AJ, Milewski KP, Buszman PP, Trendel W, Kolarczyk-Haczyk A, et al. Long Term Outcomes in Diabetic Patients Treated With Atherectomy for Peripheral Artery Disease. Cardiol J. 2018. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30394507
- Rocha-Singh KJ, Jaff MR, Crabtree TR, Bloch DA, Ansel G. Performance goals and endpoint assessments for clinical trials of femoropopliteal bare nitinol stents in patients with symptomatic peripheral arterial disease. Catheter Cardiovasc Interv. 2007; 69: 910-919. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17377972
- Kawamura Y, Ishii H, Aoyama T, Tanaka M, Takahashi H, et al. Nitinol stenting improves primary patency of the superficial femoral artery after percutaneous transluminal angioplasty in hemodialysis patients: A propensity-matched analysis. J Vasc Sur. 2009; 50: 1057-1062. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19782527
- Lindquist J, Schramm K. Drug-Eluting Balloons and Drug-Eluting Stents in the Treatment of Peripheral Vascular Disease. Semin Intervent Radiol. 2018; 35: 443–452. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30728660
- Cipollari S, Yokoi H, Ohki T, Kichikawa K, Nakamura M, et al. Long-Term Effectiveness of the Zilver PTX Drug-Eluting Stent for Femoropopliteal Peripheral Artery Disease in Patients with No Patent Tibial Runoff VesselsResults from the Zilver PTX Japan Post-Market Surveillance Study. J Vasc Interv Radiol. 2018; 29: 9-17. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29122449
- Litsky J, Chanda A, Stilp E, Lansky A, Mena C. Critical evaluation of stents in the peripheral arterial disease of the superficial femoral artery – focus on the paclitaxel eluting stent Med Device. 2014; 7: 149–156. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4045256/
- Oikonomopoulou K, Ricklin D, Ward PA, John D. Interactions between coagulation and complement—their role in inflammation. Semin Immunopathol. 2012; 34: 151–165. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21811895
Similar Articles
-
Left Atrial Remodeling is Associated with Left Ventricular Remodeling in Patients with Reperfused Acute Myocardial InfarctionChristodoulos E. Papadopoulos*,Dimitrios G. Zioutas,Panagiotis Charalambidis,Aristi Boulbou,Konstantinos Triantafyllou,Konstantinos Baltoumas,Haralambos I. Karvounis,Vassilios Vassilikos. Left Atrial Remodeling is Associated with Left Ventricular Remodeling in Patients with Reperfused Acute Myocardial Infarction. . 2016 doi: 10.29328/journal.jccm.1001001; 1: 001-008
-
Mid-Ventricular Ballooning in Atherosclerotic and Non-Atherosclerotic Abnormalities of the Left Anterior Descending Coronary ArteryStefan Peters*. Mid-Ventricular Ballooning in Atherosclerotic and Non-Atherosclerotic Abnormalities of the Left Anterior Descending Coronary Artery. . 2016 doi: 10.29328/journal.jccm.1001002; 1:
-
Concentration Polarization of Ox-LDL and Its Effect on Cell Proliferation and Apoptosis in Human Endothelial CellsShijie Liu*,Jawahar L Mehta,Yubo Fan,Xiaoyan Deng,Zufeng Ding*. Concentration Polarization of Ox-LDL and Its Effect on Cell Proliferation and Apoptosis in Human Endothelial Cells. . 2016 doi: 10.29328/journal.jccm.1001003; 1:
-
Intermittent Left Bundle Branch Block: What is the Mechanism?Hussam Ali*,Riccardo Cappato. Intermittent Left Bundle Branch Block: What is the Mechanism?. . 2017 doi: 10.29328/journal.jccm.1001004; 2:
-
Congenital Quadricuspid Aortic Valve, a Rare Cause of Aortic Insufficiency in Adults: Case ReportCyrus Kocherla*,Kalgi Modi. Congenital Quadricuspid Aortic Valve, a Rare Cause of Aortic Insufficiency in Adults: Case Report. . 2017 doi: 10.29328/journal.jccm.1001005; 2: 003-007
-
Short and Medium-Term Evaluation of Patients in Coronary Post-Angioplasty: Préliminary results at the Cardiology Department of the Hospital University Aristide Le Dantec of Dakar (Senegal): Study on 38 CasesDioum M*,Aw F,Masmoudi K,Gaye ND,Sarr SA,Ndao SCT, Mingou J,Ngaidé AA,Diack B,Bodian M,Ndiaye MB,Diao M,Ba SA. Short and Medium-Term Evaluation of Patients in Coronary Post-Angioplasty: Préliminary results at the Cardiology Department of the Hospital University Aristide Le Dantec of Dakar (Senegal): Study on 38 Cases. . 2017 doi: 10.29328/journal.jccm.1001006; 2: 008-012
-
Indications and Results of Coronarography in Senegalese Diabetic Patients: About 45 CasesNdao SCT*,Gaye ND,Dioum M,Ngaide AA,Mingou JS,Ndiaye MB, Diao M,Ba SA. Indications and Results of Coronarography in Senegalese Diabetic Patients: About 45 Cases. . 2017 doi: 10.29328/journal.jccm.1001007; 2: 013-019
-
Procedure utilization, latency and mortality: Weekend versus Weekday admission for Myocardial InfarctionNader Makki,David M Kline,Arun Kanmanthareddy,Hansie Mathelier,Satya Shreenivas,Scott M Lilly*. Procedure utilization, latency and mortality: Weekend versus Weekday admission for Myocardial Infarction. . 2017 doi: 10.29328/journal.jccm.1001008; 2: 020-025
-
Spontaneous rupture of a giant Coronary Artery Aneurysm after acute Myocardial InfarctionOğuzhan Çelik,Mucahit Yetim,Tolga Doğan,Lütfü Bekar,Macit Kalçık*,Yusuf Karavelioğlu. Spontaneous rupture of a giant Coronary Artery Aneurysm after acute Myocardial Infarction. . 2017 doi: 10.29328/journal.jccm.1001009; 2: 026-028
-
Thrombolysis, the only Optimally Rapid Reperfusion TreatmentVictor Gurewich*. Thrombolysis, the only Optimally Rapid Reperfusion Treatment. . 2017 doi: 10.29328/journal.jccm.1001010; 2: 029-034
Recently Viewed
-
Pneumothorax as Complication of CT Guided Lung Biopsy: Frequency, Severity and Assessment of Risk FactorsGaurav Raj*,Neha Kumari,Neha Singh,Kaustubh Gupta,Anurag Gupta,Pradyuman Singh,Hemant Gupta. Pneumothorax as Complication of CT Guided Lung Biopsy: Frequency, Severity and Assessment of Risk Factors. J Radiol Oncol. 2025: doi: 10.29328/journal.jro.1001075; 9: 012-016
-
The Police Power of the National Health Surveillance Agency – ANVISADimas Augusto da Silva*,Rafaela Marinho da Silva. The Police Power of the National Health Surveillance Agency – ANVISA. Arch Cancer Sci Ther. 2024: doi: 10.29328/journal.acst.1001046; 8: 063-076
-
A Comparative Study of Serum Sodium and Potassium Levels across the Three Trimesters of PregnancyOtoikhila OC and Seriki SA*. A Comparative Study of Serum Sodium and Potassium Levels across the Three Trimesters of Pregnancy. Clin J Obstet Gynecol. 2023: doi: 10.29328/journal.cjog.1001137; 6: 108-116
-
Chaos to Cosmos: Quantum Whispers and the Cosmic GenesisOwais Farooq*,Romana Zahoor*. Chaos to Cosmos: Quantum Whispers and the Cosmic Genesis. Int J Phys Res Appl. 2025: doi: 10.29328/journal.ijpra.1001107; 8: 017-023
-
Phytochemical Compounds and the Antifungal Activity of Centaurium pulchellum Ethanol Extracts in IraqNoor Jawad Khadhum, Neepal Imtair Al-Garaawi*, Antethar Jabbar Al-Edani. Phytochemical Compounds and the Antifungal Activity of Centaurium pulchellum Ethanol Extracts in Iraq. J Plant Sci Phytopathol. 2024: doi: 10.29328/journal.jpsp.1001137; 8: 079-083
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."