Abstract
Research Article
Effects of highest dose of sacubitril/valsartan association compared to lower doses on mortality and ventricular arrhythmias
Paul Milliez*, Florent Allain, Damien Legallois, Katrien Blanchart, Laure Champ-Rigot, Arnaud Pellissier, Pierre Ollitrault, Mathieu Chequel, Rémi Sabatier, Alain Lebon, Sophie Gomes, Olivier Citerne and Farzin Beygui
Published: 24 April, 2020 | Volume 5 - Issue 1 | Pages: 089-094
Background: Sudden cardiac death is a major healthcare issue in reduced ejection fraction heart failure (HFrEF) patients. Recently, the new association of sacubitril/valsartan showed a reduction of both ventricular arrhythmias (VA) and mortality even at low dose compared to enalapril in HF patients. The purpose of our study was to assess whether the highest dose of sacubitril/valsartan compared to lower doses may improve the rate of death and VA in a population of patients with HFrEF and with an implantable cardiac defibrillator (ICD).
Methods: 104 HF patients with reduced EF under sacubitril/valsartan with an ICD were divided in 2 groups: the first one with the lower doses of sacubitril/valsartan (24/26 mg or 49 mg/51 mg twice daily) and the second with the maximal dose (97mg/103mg twice daily). The primary outcome was a composite of death or appropriate ICD therapy for VA.
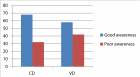
Results: After a median follow-up of 14 months, 39 patients were treated with lower doses and 65 patients with the highest dose. Patients from the lower doses group were older (70 [60-80] vs. 66 [60-70]; p = 0,03), more symptomatic at initiation (NYHA 3: 44% vs. 19%; p < 0,01) and more often in atrial fibrillation (31% vs. 12%; p = 0,04). The primary composite endpoint occurred in 14 patients (36%) in the low doses group versus 7 patients (11%) in high dose group (p < 0,01). This difference was particularly observed in the subgroup of patients with ischemic cardiomyopathy. In a multivariable analysis, the higher dose was independently associated with the primary outcome with an HR = 2,934 [IC 95% 1,147 – 7,504]; p = 0,03. Kaplan-Meier curve showed an early effect of the highest dose of sacubitril/valsartan association.
Conclusion: Patients with HFrEF under the highest dose of sacubitril/valsartan showed better clinical outcomes with a decrease of both mortality or appropriated ICD therapies related to ventricular arrhythmias.
Read Full Article HTML DOI: 10.29328/journal.jccm.1001092 Cite this Article Read Full Article PDF
Keywords:
Sacubitril/valsartan; Dose; Mortality; Ventricular arrhythmia; Implantable cardiac defibrillator
References
- Kong MH, Fonarow GC, Peterson ED, Curtis AB, Hernandez AF, et al. Systematic review of the incidence of sudden cardiac death in the United States. J Am Coll Cardiol. 2011; 57: 794-801. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21310315
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, et al. 2016. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Eur J Heart Fail. 2016; 18: 891-975. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/27207191
- McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, et al; PARADIGM-HF Investigators and Committees.Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371: 993–1004. PubMed : https://www.ncbi.nlm.nih.gov/pubmed/25176015
- Vardeny O, Claggett B, Packer M, Zile MR, Rouleau J, et al. Efficacy of sacubitril/valsartan vs.. enalapril at lower than target doses in heart failure with reduced ejection fraction: the PARADIGM-HF trial. European Journal of Heart Failure, 2016; 18: 1228–1234. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/27283779
- de Diego C, González-Torres L, Núñez JM, Centurión Inda R, Martin-Langerwerf DA, et al. Effects of angiotensin-neprilysin inhibition compared to angiotensin inhibition on ventricular arrhythmias in reduced ejection fraction patients under continuous remote monitoring of implantable defibrillator devices. Heart Rhythm. 2018; 15: 395–402. PubMed : https://www.ncbi.nlm.nih.gov/pubmed/29146274
- Wilkoff BL, Fauchier L, Stiles MK, Morillo CA, Al-Khatib SM, et al. 2015 HRS/EHRA/APHRS/SOLAECE expert consensus statement on optimal implantable cardioverter-defibrillator programming and testing. Europace. 2016; 18: 159–183. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26585598
- Webb RL, de Gasparo M. Role of the angiotensin II receptor blocker valsartan in heart failure. Exp Clin Cardiol. 2001; 6: 215-221. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2859003/
- Young JB. Mortality and Morbidity Reduction with Candesartan in Patients With Chronic Heart Failure and Left Ventricular Systolic Dysfunction: Results of the CHARM Low-Left Ventricular Ejection Fraction Trials. Circulation. 2004; 110: 2618–2626. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15492298
- Hubers SA, Brown NJ. Combined Angiotensin Receptor Antagonism and Neprilysin Inhibition. Circulation. 2016; 133: 1115–1124. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26976916
- Iborra-Egea O, Gálvez-Montón C, Roura S, Perea-Gil I, Prat-Vidal C, et al. Mechanisms of action of sacubitril/valsartan on cardiac remodeling: a systems biology approach. Npj Systems Biology and Applications. 2017; 3.
- Sarrias A, Bayes-Genis A. Is Sacubitril/Valsartan (Also) an Antiarrhythmic Drug? Circulation. 2018; 138: 551–553. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30354612
- Franz MR, Cima R, Wang D, Profitt D, Kurz R. Electrophysiological Effects of Myocardial Stretch and Mechanical Determinants of Stretch-Activated Arrhythmias. Circulation. 1992; 86: 968-978. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/1381296
Figures:
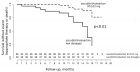
Figure 1
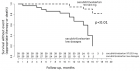
Figure 2
Similar Articles
-
Left Atrial Remodeling is Associated with Left Ventricular Remodeling in Patients with Reperfused Acute Myocardial InfarctionChristodoulos E. Papadopoulos*,Dimitrios G. Zioutas,Panagiotis Charalambidis,Aristi Boulbou,Konstantinos Triantafyllou,Konstantinos Baltoumas,Haralambos I. Karvounis,Vassilios Vassilikos. Left Atrial Remodeling is Associated with Left Ventricular Remodeling in Patients with Reperfused Acute Myocardial Infarction. . 2016 doi: 10.29328/journal.jccm.1001001; 1: 001-008
-
Indications and Results of Coronarography in Senegalese Diabetic Patients: About 45 CasesNdao SCT*,Gaye ND,Dioum M,Ngaide AA,Mingou JS,Ndiaye MB, Diao M,Ba SA. Indications and Results of Coronarography in Senegalese Diabetic Patients: About 45 Cases. . 2017 doi: 10.29328/journal.jccm.1001007; 2: 013-019
-
Procedure utilization, latency and mortality: Weekend versus Weekday admission for Myocardial InfarctionNader Makki,David M Kline,Arun Kanmanthareddy,Hansie Mathelier,Satya Shreenivas,Scott M Lilly*. Procedure utilization, latency and mortality: Weekend versus Weekday admission for Myocardial Infarction. . 2017 doi: 10.29328/journal.jccm.1001008; 2: 020-025
-
Non-hemodynamic factors associated to the risk of developing hypertensive cardiopathyAlexis Álvarez-Aliaga*,Julio César González-Aguilera,Liliana del Rosario Maceo-Gómez,Lic David del Llano Sosa,Raúl Leyva-Castro,Rosa Ojeda-Vázquez. Non-hemodynamic factors associated to the risk of developing hypertensive cardiopathy. . 2017 doi: 10.29328/journal.jccm.1001017; 2: 068-084
-
Design and validation of an Index to predict the development of Hypertensive CardiopathyAlexis Álvarez-Aliaga*,Andrés José Quesada-Vázquez,Alexis Suárez-Quesada,David de Llano Sosa. Design and validation of an Index to predict the development of Hypertensive Cardiopathy. . 2018 doi: 10.29328/journal.jccm.1001022; 3: 008-022
-
Cardiovascular damage during lupus in black African subjectsYaméogo NV*,Tougouma SJ-B,Zabsonré J,Kologo KJ,Tiemtoré WS,Kagambèga LJ,Bagbila WPAH, Traoré A,Samadoulougou AK,Zabsonré P. Cardiovascular damage during lupus in black African subjects. . 2018 doi: 10.29328/journal.jccm.1001024; 3: 031-034
-
Timing of cardiac surgery and other intervention among children with congenital heart disease: A review articleChinawa JM*,Adiele KD,Ujunwa FA,Onukwuli VO,Arodiwe I,Chinawa AT,Obidike EO,Chukwu BF. Timing of cardiac surgery and other intervention among children with congenital heart disease: A review article. . 2019 doi: 10.29328/journal.jccm.1001047; 4: 094-099
-
Prevalence of congenital heart diseases among primary school children in the Niger Delta Region of Nigeria, West AfricaUjuanbi Amenawon Susan*,Tabansi Petronilla Nnena,Otaigbe Barbara Edewele. Prevalence of congenital heart diseases among primary school children in the Niger Delta Region of Nigeria, West Africa. . 2019 doi: 10.29328/journal.jccm.1001056; 4: 144-149
-
Evaluation of the predictive value of CHA2DS2-VASc Score for no-reflow phenomenon in patients with ST-segment elevation myocardial infarction who underwent Primary Percutaneous Coronary InterventionMahmoud Shawky Abd El-Moneum*. Evaluation of the predictive value of CHA2DS2-VASc Score for no-reflow phenomenon in patients with ST-segment elevation myocardial infarction who underwent Primary Percutaneous Coronary Intervention. . 2019 doi: 10.29328/journal.jccm.1001061; 4: 171-176
-
Do beta adrenoceptor blocking agents provide the same degree of clinically convincing morbidity and mortality benefits in patients with chronic heart failure? A literature reviewMartin Mumuni Danaah Malick*. Do beta adrenoceptor blocking agents provide the same degree of clinically convincing morbidity and mortality benefits in patients with chronic heart failure? A literature review. . 2019 doi: 10.29328/journal.jccm.1001063; 4: 182-186
Recently Viewed
-
Diagnosis and Treatment of Anterior Cracked Tooth: A Case ReportWellington Luiz de Oliveira Da Rosa,Lucas Pradebon Brondani,Tiago Machado Da Silva,Evandro Piva, Fernandes Da Silva*. Diagnosis and Treatment of Anterior Cracked Tooth: A Case Report. J Clin Adv Dent. 2017: doi: 10.29328/journal.hjd.1001003 ; 1: 012-020
-
Relationship between Fertility Diet Score Index Items and Ovulation in Women with Polycystic Ovary Syndrome: A Narrative ReviewHadis Alimoradi,Faezeh Mashhadi,Ava Hemmat,Mohsen Nematy,Maryam Khosravi,Maryam Emadzadeh,Nayere Khadem Ghaebi,Fatemeh Roudi*. Relationship between Fertility Diet Score Index Items and Ovulation in Women with Polycystic Ovary Syndrome: A Narrative Review. Arch Food Nutr Sci. 2024: doi: 10.29328/journal.afns.1001061; 9: 041-048
-
Treatment Options for Congenital Dyserythropoietic Anemias (CDAs): Advances in Bone Marrow Transplantation, Gene Therapy, and Targeted TherapiesSophia Delicou*,Maria Moraki,Elena Papatheodorou,Aikaterini Xydaki. Treatment Options for Congenital Dyserythropoietic Anemias (CDAs): Advances in Bone Marrow Transplantation, Gene Therapy, and Targeted Therapies. J Hematol Clin Res. 2024: doi: 10.29328/journal.jhcr.1001031; 8: 027-033
-
Congenital Dysfibrinogenaemia: A Family Case ReportG García-Donas*,MT Vargas,C Martínez-Chinchilla,N Alkadi,A Rodríguez. Congenital Dysfibrinogenaemia: A Family Case Report. J Hematol Clin Res. 2024: doi: 10.29328/journal.jhcr.1001032; 8: 034-038
-
Laryngeal Xanthogranulomatosis: A Case ReportMicaela Redivo, María del Pilar Mingheira, Federica Fernandez Long, Carlos Santiago Ruggeri*. Laryngeal Xanthogranulomatosis: A Case Report. Heighpubs Otolaryngol Rhinol. 2024: doi: 10.29328/journal.hor.1001028; 8: 001-003
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."